Why Our Healthcare System Fails Despite Good Intentions
Why Our Healthcare System Fails Despite Good Intentions
Problems mount while solutions stall. America spends more on healthcare than any nation, yet our outcomes lag behind countries investing far less. We face a paradox where medical innovation flourishes alongside declining life expectancy and growing health disparities.
The diagnosis many experts avoid confronting is institutional capture - the process by which regulatory bodies and healthcare organizations gradually serve interests beyond their original mission. This phenomenon explains why transformative change remains elusive despite decades of reform attempts.
The Anatomy of Capture
Institutional capture in healthcare operates through multiple channels. When regulatory agencies develop symbiotic relationships with the industries they oversee, their independence erodes. The revolving door between government positions and lucrative industry roles creates natural alignment between regulators and the regulated.
Consider how pharmaceutical pricing persists as a policy challenge. Despite overwhelming public support for negotiating drug prices, meaningful action stalled for decades. The pharmaceutical industry deploys approximately 1,500 lobbyists in Washington annually, spending hundreds of millions on influence campaigns. Their effectiveness isn't necessarily through corruption but through relationship-building, information control, and shaping the boundaries of acceptable debate.
Similar dynamics play out across healthcare. Hospital consolidation continues despite evidence that it raises prices without improving quality. Insurance markets remain concentrated in many regions. Medical device regulation follows patterns benefiting incumbent manufacturers. The common thread is that institutions designed to protect public health gradually orient toward maintaining industry stability instead.
Beyond Simple Villains
The temptation to identify villains misses the structural nature of the problem. Healthcare executives, pharmaceutical researchers, and insurance administrators generally believe in their mission to improve health. Most regulators genuinely aim to protect the public while balancing innovation and safety.
Institutional capture happens not through malice but through incremental shifts in perspective, incentives, and organizational culture. When healthcare leaders spend more time with investors than patients, priorities change. When regulatory success gets measured by approval speed rather than public health outcomes, standards evolve accordingly.
The result is a system where good people working within captured institutions produce suboptimal results. This explains why well-intentioned reforms often disappoint. The Affordable Care Act expanded coverage significantly yet did little to address fundamental cost drivers or quality issues. Bipartisan legislation to increase transparency has yielded minimal practical impact on patient costs.
Reclaiming Our Health Institutions
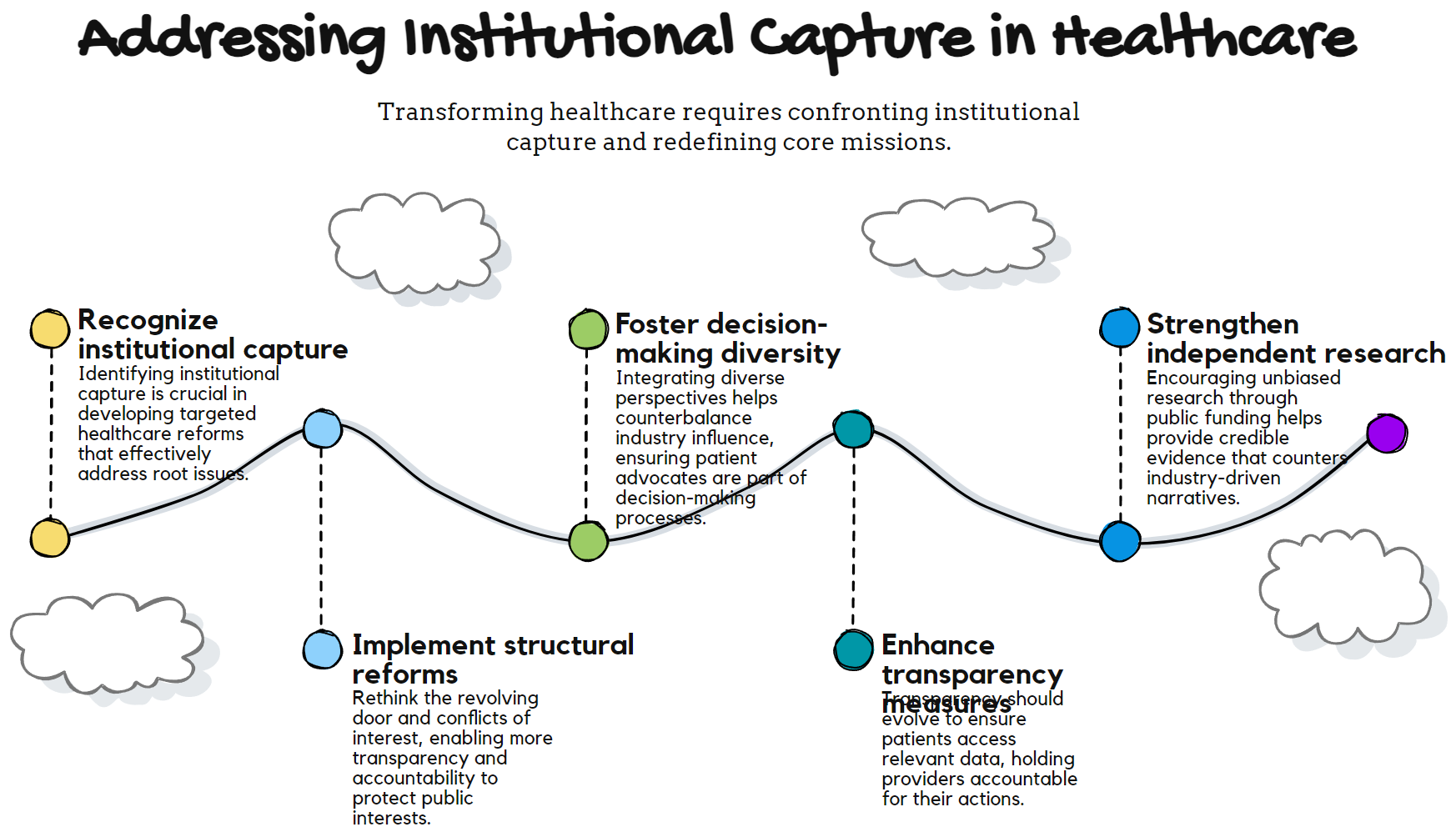
Meaningful reform requires recognizing institutional capture as a central challenge rather than a peripheral concern. Several pathways could help reclaim healthcare institutions for their public purpose.
First, structural reforms must systematically address conflicts of interest. This means rethinking the revolving door between industry and regulatory positions, strengthening disclosure requirements, and creating stronger counterweights to industry influence in policy development.
Second, we need greater diversity in decision-making bodies. Capturing becomes more difficult when FDA advisory committees, hospital boards, and health policy teams include robust representation from patient advocates, public health experts, and frontline clinicians. Diverse perspectives create natural resistance to narrow interests.
Third, transparency must evolve beyond disclosure to meaningful accountability. Publishing data on pharmaceutical company payments to doctors or hospital prices accomplishes little if this information remains functionally inaccessible to patients or lacks consequences for providers.
Fourth, we should strengthen independent research capacity. Knowledge becomes captured when evidence about healthcare interventions comes predominantly from industry-funded studies. Expanding public funding for comparative effectiveness research and health systems evaluation provides an essential counterbalance.
The Courage to Reform
Addressing institutional capture requires political courage. Powerful interests will resist substantive changes threatening established business models or regulatory relationships. Reform advocates face sophisticated opposition from entities with resources to shape the public narrative and political incentives.
Yet examples from other sectors and countries demonstrate that reclaiming captured institutions remains possible. After the 2008 financial crisis, banking regulation transformed when public pressure overcame industry resistance. Several European nations have implemented healthcare reforms that maintain innovation while controlling costs more effectively than the American system.
The path forward starts with clearly naming the problem. When discussing healthcare solely through the lens of coverage, technology, or finance, we miss the institutional dynamics perpetuating dysfunction. By recognizing capture as a central challenge, we can design reforms that address root causes rather than symptoms.
A System Worthy of Its Mission
Healthcare institutions exist to serve human health and well-being. When they drift from this purpose, the consequences appear in statistics but manifest in human suffering. Every preventable complication, unaffordable treatment, or medical bankruptcy represents institutional failure.
Americans deserve a healthcare system in which institutions remain true to their core mission. This means regulatory bodies that prioritize public health over industry relationships, hospital systems that optimize for patient outcomes rather than revenue cycles, and research enterprises that pursue knowledge benefiting humanity rather than quarterly returns.
Creating such a system requires more than technical solutions or incremental adjustments. It demands recommitment to the principle that healthcare institutions exist to serve patients and communities first. By confronting institutional capture directly, we open the possibility of reforms that deliver on the promise of better health for all Americans.
