The Forgotten Art of Medication Deprescription
The Forgotten Art of Medication Deprescription
Doctors learn to prescribe medications, but few are taught when or how to take patients off them.
Our healthcare system excels at addition. New symptoms? Add a medication. Side effects from that medication? Add another to counter them. Blood sugar still high? Increase the dose or add insulin.
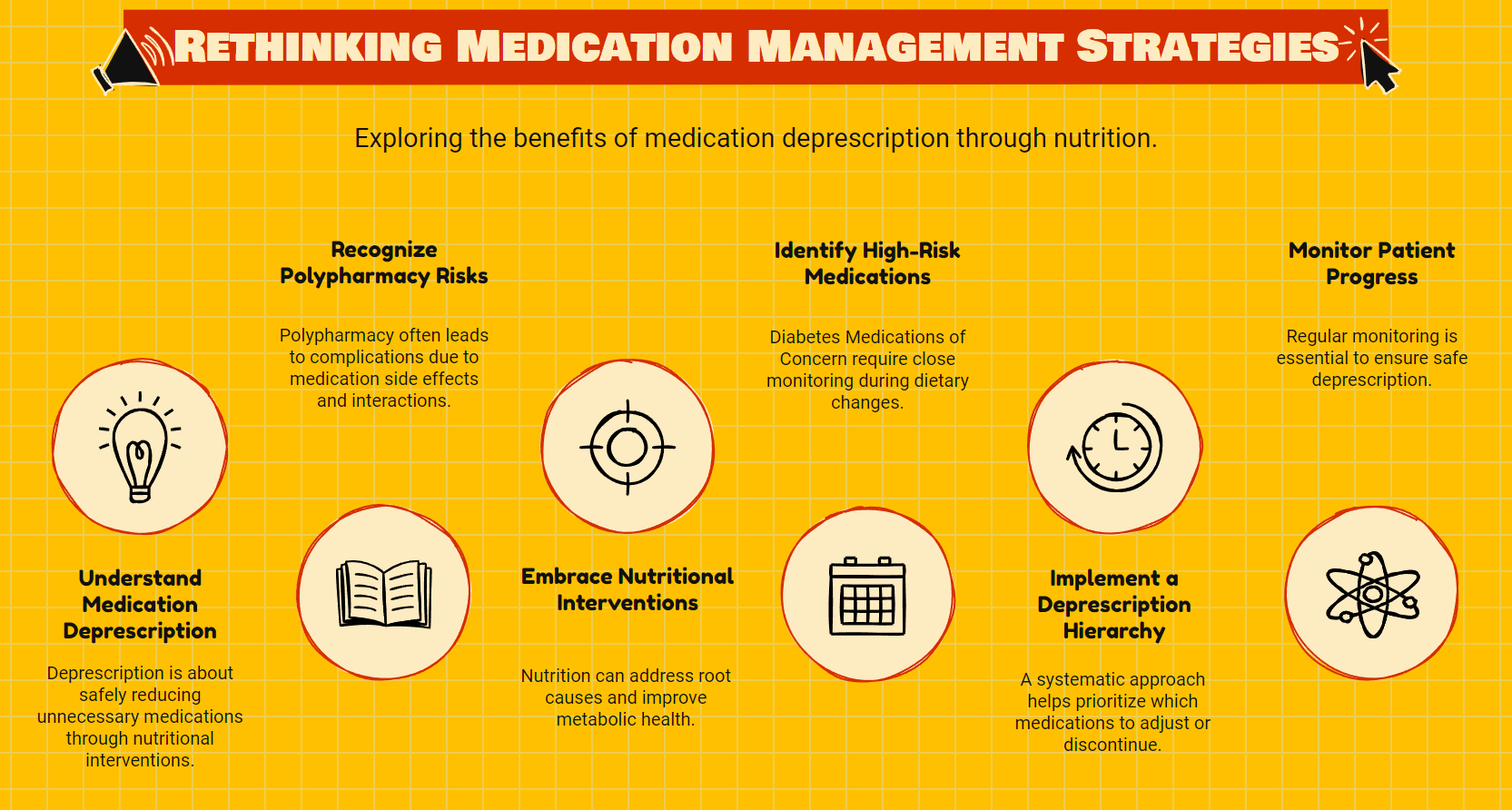
This approach has created a polypharmacy epidemic, with patients often taking multiple medications with compounding side effects and interactions. Yet there's an alternative path gaining traction that challenges this paradigm: medication deprescription through nutritional intervention.
The concept is simple but revolutionary. What if, instead of managing chronic conditions with an ever-expanding medication regimen, we could address the root cause through nutrition and safely remove unnecessary medications?
Redefining Deprescription
Currently, the medical community narrowly defines deprescribing as reducing inappropriate medications in elderly patients with polypharmacy. This definition misses something crucial.
A second definition worth fighting for is "I don't need it anymore."
This represents a fundamental shift in how we think about chronic disease management. Rather than accepting medication dependence as inevitable, it positions certain medications as temporary interventions that can be reduced or eliminated when the underlying condition improves.
This approach is particularly relevant for type 2 diabetes and metabolic disorders, where low-carbohydrate nutrition has shown remarkable results in improving metabolic health and reducing medication requirements.
The Science Behind Medication Reduction
Research consistently demonstrates that low-carbohydrate dietary approaches are as effective as or superior to other dietary approaches for type 2 diabetes management. Studies show greater reductions in diabetes medication requirements in lower-carbohydrate groups.
The mechanism is straightforward: carbohydrate restriction reduces blood glucose excursions, decreasing the need for glucose-lowering medications.
What's surprising is how quickly this happens. Patients often experience significant improvements in blood glucose levels within days of starting a low-carbohydrate diet, necessitating immediate medication adjustments to prevent hypoglycemia.
This rapid response creates both an opportunity and a challenge. The opportunity is the potential for a dramatic reduction in medication burden. The challenge is ensuring this process happens safely.
Diabetes Medications of Concern (DMOCs)
Not all medications carry equal risk during the transition to a low-carbohydrate diet. Some require immediate attention and careful monitoring.
The highest priority medications to address are what can be called "Diabetes Medications of Concern" or DMOCs. These medications can cause dangerous side effects when continued alongside carbohydrate restriction.
SGLT2 Inhibitors
SGLT2 inhibitors (medications like empagliflozin, canagliflozin, and dapagliflozin) present perhaps the most serious risk. When combined with carbohydrate restriction, they can trigger a dangerous condition called euglycemic diabetic ketoacidosis (euDKA).
This condition is insidious because blood glucose levels may appear normal or only slightly elevated, leading to delayed diagnosis. During periods of carbohydrate restriction, SGLT2 inhibitor therapy can promote lipolysis and ketogenesis while maintaining regular blood sugar, creating a perfect storm for euDKA.
The safest approach is discontinuing SGLT2 inhibitors at least three days before beginning carbohydrate restriction.
Insulin and Insulin Secretagogues
Insulin and medications that increase insulin secretion (like sulfonylureas) carry a high risk of hypoglycemia when continued at the same dose during carbohydrate restriction.
Practical expertise suggests a 50% reduction of daily insulin dose at initiation of a low-carb diet is appropriate in most cases. For patients with markedly elevated HbA1c, a more minor reduction of perhaps 30% may be applicable, with further reductions over time.
Prandial (mealtime) insulin typically must be reduced first and most aggressively, often eliminated within days of starting carbohydrate restriction.
Similarly, sulfonylureas (like glipizide, glyburide, and glimepiride) need prompt reduction or discontinuation to prevent dangerous hypoglycemic episodes.
The Deprescription Hierarchy
Beyond the high-risk medications, there's a general hierarchy to medication deprescribing that balances safety with optimization:
First Tier (Immediate Action Required)
- SGLT2 inhibitors
- Prandial insulin
- Sulfonylureas
Second Tier (Adjust Based on Glucose Monitoring)
- Basal insulin
- Thiazolidinediones
Third Tier (Consider Based on Individual Response)
- GLP-1 agonists
- DPP-4 inhibitors
Fourth Tier (Patient-Centered Decision)
- Metformin
This hierarchy isn't rigid but provides a framework for approaching description systematically.
The Metformin Question
Metformin deserves special consideration. Unlike other diabetes medications, metformin carries minimal hypoglycemia risk and offers potential benefits beyond glucose control, including possible cancer prevention effects and longevity benefits.
Additionally, metformin has been shown to prevent the progression to type 2 diabetes in high-risk individuals. Patients who have had type 2 diabetes remain at high risk for recurrence, even after achieving normal blood glucose through dietary intervention.
This creates an essential ethical consideration: should metformin be automatically discontinued when blood glucose normalizes, or should the decision be individualized?
The patient-centered approach suggests having an informed discussion about the risks and benefits, allowing the patient to make the final decision rather than applying a one-size-fits-all protocol.
Beyond Diabetes Medications
The deprescription process often extends beyond diabetes medications. As metabolic health improves, many patients experience improvements in blood pressure, reflux symptoms, and inflammatory conditions.
Blood pressure medications typically don't require immediate adjustment but should be monitored closely, with reductions made if orthostatic symptoms (dizziness upon standing) develop.
Proton pump inhibitors (PPIs) for reflux can often be gradually reduced as symptoms improve, though this process typically takes months rather than days.
The broader implication is that nutritional intervention can address multiple chronic conditions simultaneously, potentially reducing medication burden across several categories.
The Essential Role of Monitoring
Safe deprescription requires vigilant monitoring, especially in the early stages. This includes:
- Daily blood glucose monitoring, multiple times per day
- Regular blood pressure checks for those on antihypertensive medications
- Awareness of symptoms that might indicate medication adjustment is needed
- Regular laboratory follow-up to track longer-term markers
Monitoring intensity can decrease once high-risk medications have been appropriately adjusted or discontinued, but ongoing surveillance remains essential.
A Team Approach to Deprescription
Successful deprescription rarely happens in isolation. It requires collaboration between:
- The patient, who must be educated and engaged in the process
- Primary care providers who oversee the overall medication regimen
- Specialists who manage specific conditions
- Nutrition professionals who guide the dietary intervention
Communication between team members is crucial, especially when multiple providers are involved in a patient's care.
The Future of Deprescription
As evidence for the effectiveness of nutritional interventions grows, deprescription should become a more recognized and valued medical skill.
This requires several shifts in the medical system:
- Medical education that includes deprescribing protocols
- Clinical guidelines that acknowledge nutrition as a primary intervention
- Reimbursement systems that reward medication optimization rather than just disease management
- Research that evaluates deprescribing outcomes
The goal isn't to eliminate all medications—many provide crucial benefits that cannot be achieved through lifestyle alone. Rather, it's to ensure that each medication a patient takes offers meaningful benefits that outweigh its risks and costs.
The Patient Experience
For patients, the deprescription journey often represents more than just taking fewer pills. It means a shift from passive disease management to active health creation.
The psychological impact of reducing or eliminating medications can be profound. Patients often report a sense of empowerment and hope that had been missing in their chronic disease experience.
This emotional component shouldn't be underestimated. It can fuel the motivation to sustain dietary changes and engage more deeply in overall health improvement.
A New Definition of Optimization
True human optimization isn't about adding more interventions—whether medications, supplements, or procedures—sometimes, it's about subtraction.
By removing unnecessary medications through nutritional intervention, we address root causes rather than symptoms, reduce side effect burden, and empower patients to take control of their health.
This represents a fundamental shift from the conventional healthcare disease management model to one of health creation.
The art of deprescription deserves recognition not as a fringe concept, but as an essential component of truly patient-centered care.
