The Cholesterol Myth That Could Change Medicine Forever
The Cholesterol Myth That Could Change Medicine Forever
Beliefs can kill. What we accept as medical truth guides our choices, shapes health policies, and determines which pills we swallow each morning. For decades, the cholesterol narrative has dominated heart disease prevention. But what if this foundational pillar of modern medicine stands on shaky ground?
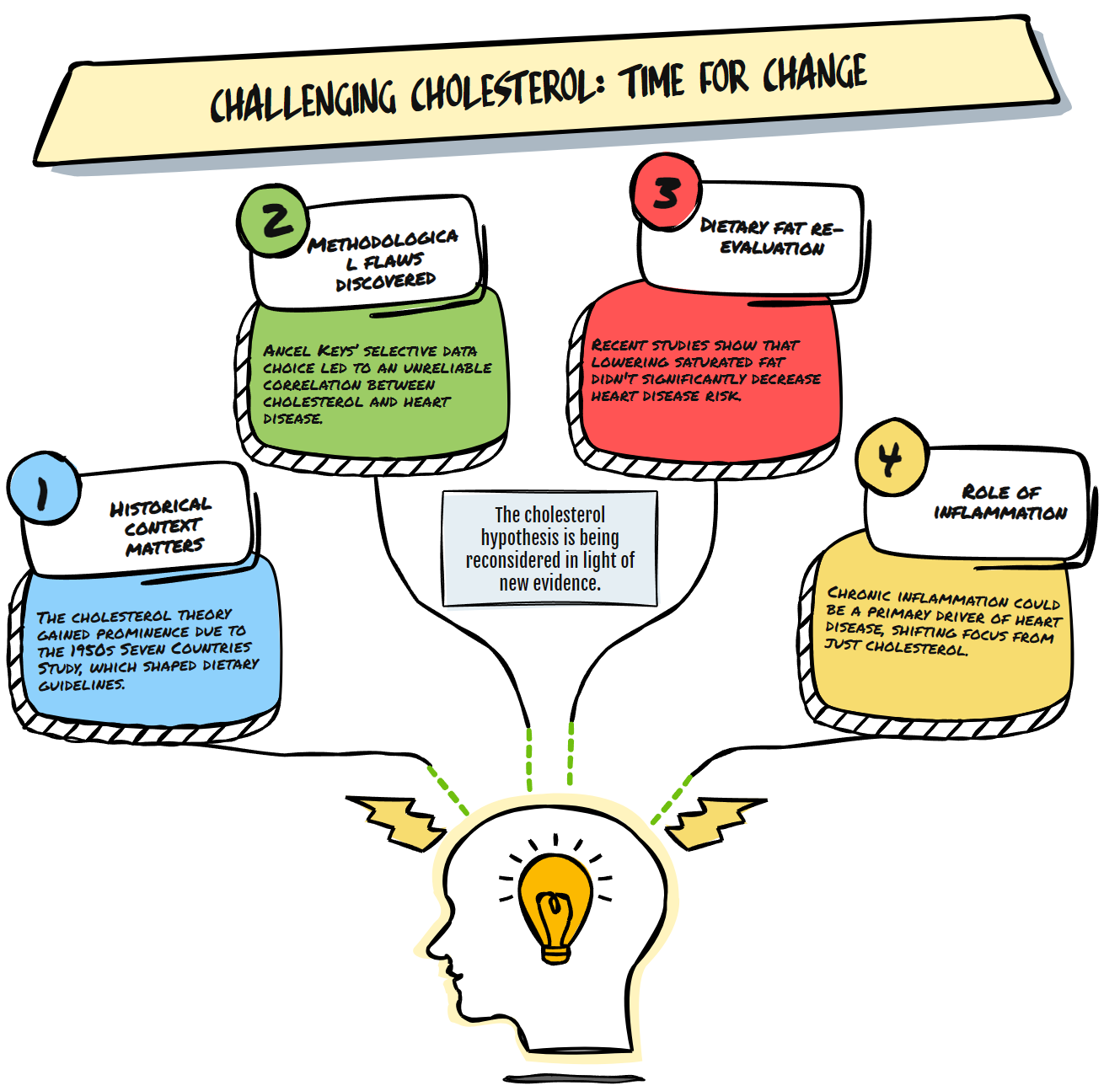
The story begins in the 1950s. America faced a heart disease epidemic with no apparent cause. Enter Ancel Keys and his Seven Countries Study, which showed a neat correlation between saturated fat consumption, cholesterol levels, and heart disease rates. This became the lipid hypothesis – the idea that dietary fat raises blood cholesterol, which then causes heart disease.
This hypothesis transformed into dogma. Food manufacturers removed fat from products. Doctors prescribed statins by the millions. Government guidelines warned against eggs, butter, and meat. An entire medical-industrial complex grew around measuring, monitoring, and medicating cholesterol.
But science moves forward. And the evidence challenging this paradigm has grown too substantial to ignore.
When Good Science Goes Bad
The original research linking cholesterol to heart disease suffered from serious methodological flaws. Keys selected countries that fit his hypothesis while excluding those that contradicted it. When researchers later analyzed data from all 22 countries available to Keys, the correlation nearly disappeared.
More troubling is that multiple large-scale studies have failed to demonstrate that lowering cholesterol through diet significantly reduces heart attack risk. The Minnesota Coronary Experiment, a randomized controlled trial conducted between 1968 and 1973 but not fully analyzed until 2016, found that participants who reduced saturated fat actually had higher mortality rates despite lowering their cholesterol.
The Women's Health Initiative, which cost $700 million and followed nearly 49,000 women for eight years, found no reduction in heart disease from a low-fat diet. These aren't fringe findings. They represent gold-standard research that contradicts what most doctors still tell patients.
The Inflammation Revolution
As the cholesterol hypothesis falters, alternative explanations have gained traction. Many researchers now believe chronic inflammation drives atherosclerosis more than cholesterol itself. This would explain why half of heart attack victims have normal cholesterol levels, while many people with high cholesterol never develop heart disease.
Numerous factors can trigger inflammation, including processed foods, environmental toxins, chronic stress, autoimmune conditions, and infectious agents. This broader view acknowledges the complexity of cardiovascular disease rather than reducing it to a single marker.
Insulin resistance represents another compelling pathway. When cells become resistant to insulin, metabolic dysfunction follows, affecting how the body processes fats and carbohydrates. This metabolic perspective helps explain why diabetes dramatically increases heart disease risk, independent of cholesterol levels.
The Statin Question
Statins remain the most prescribed class of medications worldwide. Their effectiveness in secondary prevention (preventing a second heart attack) seems clear. However, their value in primary prevention (for people who've never had heart problems) remains controversial.
The absolute risk reduction from taking statins for primary prevention is typically 1-2% over five years. Doctors must treat 50-100 people for years to prevent one cardiovascular event. Meanwhile, side effects like muscle pain, cognitive issues, and increased diabetes risk affect a significant percentage of users.
This unfavorable risk-benefit ratio rarely enters doctor-patient conversations. Most patients receive their cholesterol numbers without context about what they mean for their risk.
Beyond Simple Narratives
Medical paradigms shift slowly. Too many careers, research grants, and pharmaceutical profits depend on the status quo. But patients deserve better than outdated science.
A more nuanced approach would recognize that:
Cardiovascular disease develops through multiple pathways, not just elevated LDL.
Risk assessment should include inflammation markers, insulin sensitivity, triglyceride/HDL ratio, and lipoprotein particle size and number.
For many people, lifestyle interventions addressing sleep, stress, nutrition, and movement may provide greater benefit than medication.
Different dietary approaches work for individuals based on genetics, microbiome, and metabolic health.
The Path Forward
Questioning the cholesterol hypothesis doesn't mean ignoring heart disease risk. Instead, it means expanding our understanding beyond simplistic models that reduce complex biological systems to single variables.
Progressive clinicians now look at the whole patient. They consider metabolic health, inflammatory status, genetic factors, and lifestyle patterns. They recognize coronary disease develops over decades through multiple mechanisms, not just cholesterol accumulation.
For patients, this paradigm shift offers both responsibility and hope. It means moving beyond the false security of "normal" cholesterol numbers toward a deeper understanding of cardiovascular health. It means recognizing that nutrition science extends beyond fat grams and cholesterol counts.
Scientific progress requires questioning established beliefs, especially those that have become so ingrained that we no longer see them as theories but as facts. The cholesterol hypothesis has dominated medicine for over half a century. Its reconsideration represents not a rejection of science but science working as intended—self-correcting, evolving, and refining our understanding of human health.
The most significant risk now would be clinging to outdated models while ignoring emerging evidence. Patients deserve treatments based on current science, not historical momentum. The cholesterol controversy reminds us that in medicine, as in all scientific endeavors, questioning established wisdom often leads to better answers.
