The Brain Fuel Revolution Your Doctor Won't Tell You About
The Brain Fuel Revolution Your Doctor Won't Tell You About
Your brain is starving. Not for calories, but for the right metabolic fuel.
For decades, conventional wisdom has insisted that our brains require glucose as their primary energy source. This narrative has shaped everything from psychiatric medication approaches to dietary recommendations for mental health conditions.
But what if this fundamental assumption is wrong?
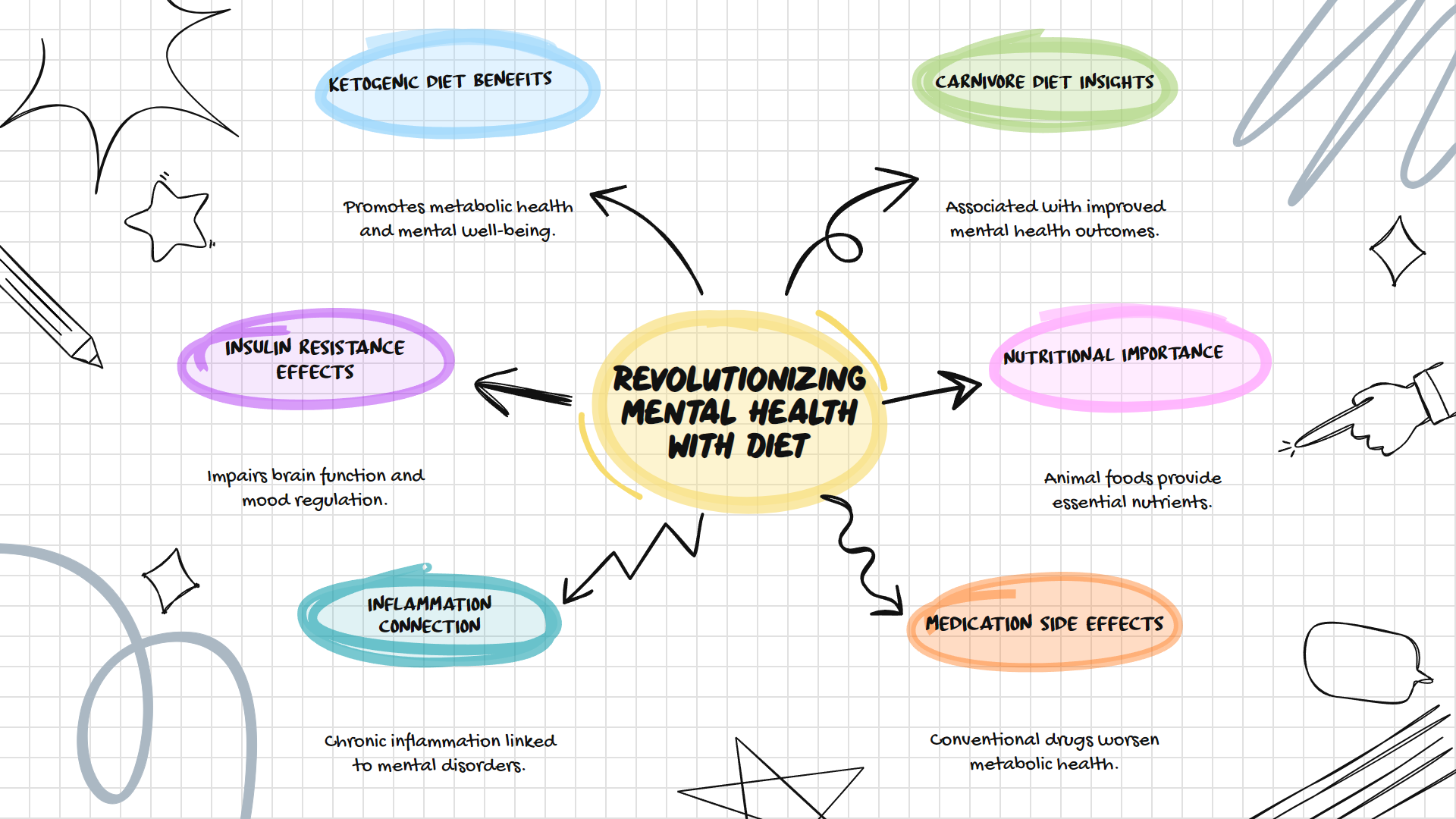
Emerging research reveals a profound connection between metabolic health and mental wellbeing that challenges our most basic understanding of psychiatric disorders. The evidence suggests that ketogenic and carnivore diets might offer powerful interventions for conditions ranging from depression to schizophrenia.
The Metabolic Roots of Mental Illness
Mental health conditions share striking biological similarities with metabolic disorders. This isn't coincidental.
Scientists have discovered that serious mental illnesses like schizophrenia, major depression, and bipolar disorder exhibit notable biological similarities with conditions successfully treated by ketogenic diets: inflammation in the brain, oxidative stress, mitochondrial dysfunction, and disrupted glucose metabolism. These aren't separate problems but interconnected metabolic disturbances affecting brain function.
The connection becomes clearer when examining how our brains process energy.
While glucose has long been considered the brain's exclusive fuel, research confirms that ketones can provide up to 75% of the brain's energy needs. For individuals with compromised glucose metabolism or insulin resistance in the brain, this alternative fuel source becomes crucial.
Insulin Resistance in the Brain
Brain insulin resistance differs from peripheral insulin resistance. The distinction matters tremendously.
In the brain, insulin resistance primarily occurs at the blood-brain barrier. When this happens, insulin can't effectively enter the brain, yet glucose continues flowing in unrestricted. This creates a dangerous situation where brain cells are swimming in glucose they cannot properly utilize.
The consequences are serious and far-reaching.
Chronic exposure to elevated glucose without proper insulin signaling leads to glycation of brain cells, triggering inflammation and oxidative stress. These processes directly contribute to cognitive impairment, mood disorders, and potentially more severe psychiatric conditions.
This metabolic disruption creates a perfect storm for mental health problems.
Clinical Evidence for Ketogenic Interventions
The theoretical foundation is compelling, but what about real-world evidence?
A recent Stanford Medicine pilot study found that ketogenic diets not only restore metabolic health in patients with serious mental illness while on antipsychotic medications but also significantly improve their psychiatric conditions. Three-quarters of participants showed clinically meaningful improvement in their mental health symptoms.
These findings aren't isolated.
In a French hospital study, 31 patients with treatment-resistant mental illness (major depression, bipolar disorder, schizophrenia) were treated with a ketogenic diet. Results showed 64% of patients were discharged on less psychiatric medication, and 43% achieved clinical remission, suggesting significant therapeutic potential for conditions that typically respond poorly to conventional treatments.
The implications challenge our entire approach to mental health treatment.
Carnivore Diet and Mental Health
While ketogenic diets have gained scientific attention, the carnivore diet represents a more recent and radical approach that eliminates all plant foods.
The evidence, while primarily observational at this stage, appears promising.
A survey of 2,029 adults following a carnivore diet reported substantial improvements in physical and mental well-being, overall health, and numerous chronic medical conditions. Those with diabetes reported especially significant benefits, including greater weight loss than the overall group and marked reductions in diabetes medication usage.
Another survey of 122 people following a carnivore diet found 74% reported significant improvements in their mental health, 14% reported moderate improvements, 7% mild improvements, and only 5% saw no change. No respondents reported a decline in mental health.
Most interestingly, many hadn't started the diet for mental health reasons at all. The benefits came as an unexpected bonus.
The Nutritional Connection
Why might animal-based diets benefit mental health? The answer lies in both what they provide and what they eliminate.
Animal foods contain critical nutrients that either don't exist in plant foods or exist in forms that are significantly less bioavailable. These include vitamin B12, choline, creatine, carnitine, taurine, and highly bioavailable forms of zinc, iron, and omega-3 fatty acids.
These nutrients aren't just helpful for brain function. They're essential.
A comprehensive meta-analysis published in Critical Reviews in Food Science and Nutrition analyzed 20 studies with 171,802 participants and found that meat consumption was associated with lower depression and anxiety compared to meat abstention. The analysis showed that the more rigorous the study, the more positive and consistent the relationship between meat consumption and better mental health.
Simultaneously, eliminating processed carbohydrates and plant compounds that may trigger inflammation provides a second mechanism of benefit.
The Inflammation Connection
Chronic inflammation represents a common thread linking metabolic dysfunction and mental health disorders.
Consumption of refined carbohydrates triggers systemic inflammation that can compromise the blood-brain barrier and impair neurological function. This inflammation directly impacts neurotransmitter systems implicated in mood regulation.
By eliminating inflammatory triggers, ketogenic and carnivore diets may help restore proper brain function.
Dr. Chris Palmer, Harvard psychiatrist and researcher, explains that ketogenic diets can "reduce brain inflammation, change gene expression, and actually change the gut microbiome in beneficial ways that affect the brain." When treating patients with psychiatric conditions, he typically aims for specific blood ketone levels: at least 0.8 for depression and greater than 1.5 for psychotic disorders and bipolar disorder.
Beyond Ketones
While ketones receive significant attention, the benefits of these dietary approaches likely extend beyond ketone production alone.
Insulin stabilization represents a critical mechanism. Studies have found that insulin resistance in the brain may be linked to mental health disorders. In a clinical trial on patients with treatment-resistant bipolar depression who also had insulin resistance, half of those who took the diabetes drug metformin had reversed their insulin resistance and experienced dramatic improvements in their psychiatric symptoms, even after 25 years of illness without remission.
This suggests that addressing metabolic dysfunction directly impacts mental health outcomes.
Additionally, elimination of potential inflammatory triggers from the diet may benefit individuals with sensitivities that affect neurological function. The simplified nature of carnivore diets makes them particularly effective elimination protocols.
The Medication Paradox
Perhaps the most troubling aspect of conventional psychiatric treatment is that many medications prescribed for mental health conditions actively worsen metabolic health.
Antipsychotics, commonly prescribed for conditions ranging from schizophrenia to bipolar disorder and increasingly for anxiety and insomnia, are notorious for causing weight gain, insulin resistance, and metabolic syndrome. These side effects aren't merely cosmetic concerns but directly impact the same metabolic pathways implicated in the mental health conditions they aim to treat.
This creates a vicious cycle where treatment worsens the underlying metabolic dysfunction.
By contrast, ketogenic and carnivore diets address these metabolic factors directly, potentially allowing for reduced medication needs and fewer side effects.
Implementation Considerations
Despite promising evidence, these dietary approaches aren't one-size-fits-all solutions.
Different individuals may benefit from various implementations ranging from classic ketogenic diets (4:1 or 3:1 fat-to-protein ratios) to more moderate approaches (2:1 or 1:1 ratios) or carnivore variations. Some may benefit from cyclical approaches or the inclusion of specific plant foods based on individual tolerance.
Importantly, individuals on psychiatric medications should never discontinue them without medical supervision.
The optimal approach involves working with healthcare providers who understand both the metabolic aspects of mental health and the potential of dietary interventions. Unfortunately, such providers remain relatively rare in conventional medical settings.
The Path Forward
The connection between metabolism and mental health represents one of the most promising frontiers in psychiatric research.
As research continues to validate these approaches, we may see a fundamental shift in how mental health conditions are understood and treated. Rather than viewing psychiatric disorders as primarily neurotransmitter imbalances requiring pharmaceutical correction, we might increasingly recognize them as manifestations of metabolic dysfunction amenable to dietary intervention.
This perspective doesn't dismiss the complexity of mental health or the value of conventional treatments for many individuals. Instead, it adds a powerful new dimension to our understanding and treatment options.
For those suffering from treatment-resistant mental health conditions or those experiencing metabolic side effects from psychiatric medications, ketogenic and carnivore diets offer evidence-based alternatives worth serious consideration.
The brain fuel revolution isn't just about changing what we eat. It's about fundamentally reconceptualizing mental health through the lens of metabolism.
Your brain isn't just what you think. It's what you feed it.
