Reclaiming Your Metabolic Health Before It's Too Late
Reclaiming Your Metabolic Health Before It's Too Late
Bodies break. Systems fail. Metabolism crashes.
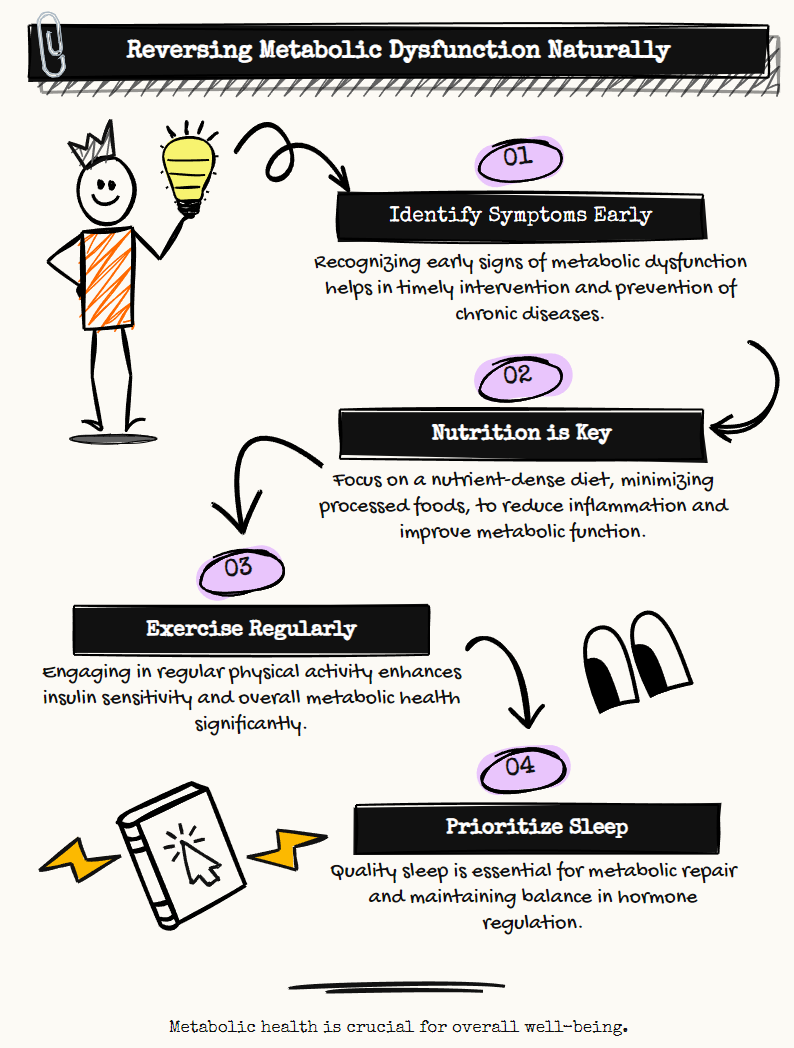
The silent epidemic of metabolic dysfunction affects far more people than most realize. Even individuals with "normal" weight can harbor serious metabolic issues that set the stage for chronic disease. The conventional healthcare approach often waits until problems manifest as diagnosable conditions before intervening, but by then, significant damage has already occurred.
What if we could identify and reverse metabolic dysfunction before it progresses to disease? The evidence suggests we can, and the solution lies not in more medications but in fundamental lifestyle interventions that address the root causes.
Understanding the Metabolic Crisis
Metabolic health represents your body's ability to properly process food into energy, regulate blood glucose, manage lipids, and balance hormones without excessive inflammation. When these systems falter, the consequences cascade throughout the body.
The warning signs often hide in plain sight: expanding waist circumference, creeping blood pressure readings, gradually rising fasting glucose, decreasing HDL cholesterol, and elevating triglycerides. These markers, collectively known as metabolic syndrome when present together, signal a body struggling to maintain homeostasis.
Most concerning is how these dysfunctions create fertile ground for chronic diseases. Type 2 diabetes, cardiovascular disease, non-alcoholic fatty liver disease, certain cancers, and even neurodegenerative conditions like Alzheimer's share metabolic dysfunction as a common denominator. Recent research has even demonstrated that COVID-19 outcomes worsen significantly in those with poor metabolic health.
Nutrition as the Foundation
The modern food environment bears little resemblance to what humans evolved consuming. Ultra-processed foods now dominate many diets, delivering calorie-dense, nutrient-poor combinations that disrupt metabolic function at the cellular level.
Restoring metabolic health begins with nutrition that reduces inflammation and insulin resistance. Low-carbohydrate approaches have demonstrated remarkable clinical success in reversing metabolic dysfunction. These dietary patterns prioritize nutrient-dense whole foods while eliminating the ultra-processed products that dominate supermarket shelves.
Contrary to decades of misguided advice, dietary fat itself is not the villain. Quality matters tremendously. Processed seed oils high in omega-6 fatty acids promote inflammation, while natural fats from animals and certain plants support cellular integrity and hormone production. Protein requirements often exceed conventional recommendations, particularly for maintaining muscle mass during weight loss.
The ideal dietary approach varies between individuals. Some thrive on ketogenic or carnivore approaches, while others do well with Mediterranean-style eating patterns. The common thread is minimizing processed foods, refined carbohydrates, and industrial oils while emphasizing whole, unprocessed options.
Movement as Medicine
Physical activity fundamentally alters metabolic function. Beyond calorie expenditure, exercise enhances insulin sensitivity, improves mitochondrial efficiency, supports hormonal balance, and reduces inflammation. The benefits extend far beyond aesthetic changes.
Strength training deserves special attention for metabolic health. Building and maintaining muscle mass creates metabolic resilience, improves glucose disposal, and supports longevity. Even modest resistance training twice weekly produces significant metabolic improvements.
High-intensity interval training (HIIT) offers another powerful intervention, creating metabolic adaptations that persist long after the workout ends. For those beginning their fitness journey, simply reducing sedentary time through walking and basic movement yields substantial benefits.
Sleep as Restoration
Sleep deprivation wreaks havoc on metabolic health. Even a single night of poor sleep increases insulin resistance, elevates stress hormones, and triggers inflammatory responses. Chronic sleep insufficiency correlates strongly with obesity, diabetes, and cardiovascular disease.
Optimizing sleep hygiene represents a no-cost, high-impact intervention. Consistent sleep-wake schedules, limiting blue light exposure before bed, maintaining cool sleeping environments, and managing evening stress all support restorative sleep. The standard recommendation of 7-9 hours reflects the time needed for metabolic repair processes.
For those struggling with sleep apnea, which severely impacts metabolic health, proper diagnosis and treatment can produce dramatic improvements in overall metabolic function.
Stress Management as Protection
Chronic psychological stress triggers physiological responses that directly impair metabolic function. Elevated cortisol promotes abdominal fat storage, increases blood glucose, and drives food cravings, particularly for calorie-dense, nutrient-poor options.
Effective stress management techniques include mindfulness meditation, deep breathing exercises, time in nature, and nurturing social connections. These practices measurably reduce inflammatory markers and improve insulin sensitivity. Even brief daily meditation sessions can significantly impact metabolic markers.
Monitoring for Mastery
Technology now enables unprecedented insight into personal metabolic responses. Continuous glucose monitors reveal real-time effects of food choices, sleep quality, stress, and exercise. Regular tracking of basic metrics like waist circumference, blood pressure, and blood markers provides feedback on intervention effectiveness.
This data-informed approach allows for personalization beyond generic recommendations. The optimal diet, exercise regimen, and lifestyle practices vary between individuals based on genetics, microbiome composition, hormonal status, and personal history.
The Path Forward
Improving metabolic health requires addressing multiple interconnected systems simultaneously. The NEST framework (Nutrition, Exercise, Sleep, Trauma/stress) provides a comprehensive approach that recognizes these connections.
Small, sustainable changes yield compounding benefits over time. Starting with nutrition typically provides the most leverage, but any improvement in sleep, stress management, or physical activity creates positive momentum.
The conventional healthcare system remains largely reactive, intervening only after disease manifests. A proactive approach focused on optimizing metabolic function offers a pathway to prevent chronic disease rather than merely managing its symptoms.
The science is clear. Metabolic health forms the foundation of overall health and longevity. By understanding and addressing the fundamental drivers of metabolic dysfunction, we can reclaim control over our health trajectory and potentially reverse conditions once considered progressive and irreversible.
The question isn't whether we can improve metabolic health through lifestyle interventions. The evidence overwhelmingly confirms we can. The real question is whether we will prioritize these approaches before metabolic dysfunction progresses to disease. Your body's answer matters more than you might think.
