Medical Nutrition Myths That Damage Your Metabolic Health
Medical Nutrition Myths That Damage Your Metabolic Health
Doctors give advice, and patients follow. This simple exchange has shaped our understanding of nutrition and health for decades. But what if the nutritional guidance coming from medical authorities isn't just ineffective but actively harmful to our metabolic health?
The metabolic health crisis facing modern society demands we reconsider conventional wisdom. With over 88% of Americans showing signs of metabolic dysfunction according to research from the University of North Carolina, we can no longer afford to follow nutritional dogma without question.
The problem runs deeper than individual food choices. It's embedded in the very framework of nutritional science and how medical professionals interpret and communicate dietary guidelines. Let's examine how conventional nutrition advice may undermine our metabolic health and what the evidence suggests.
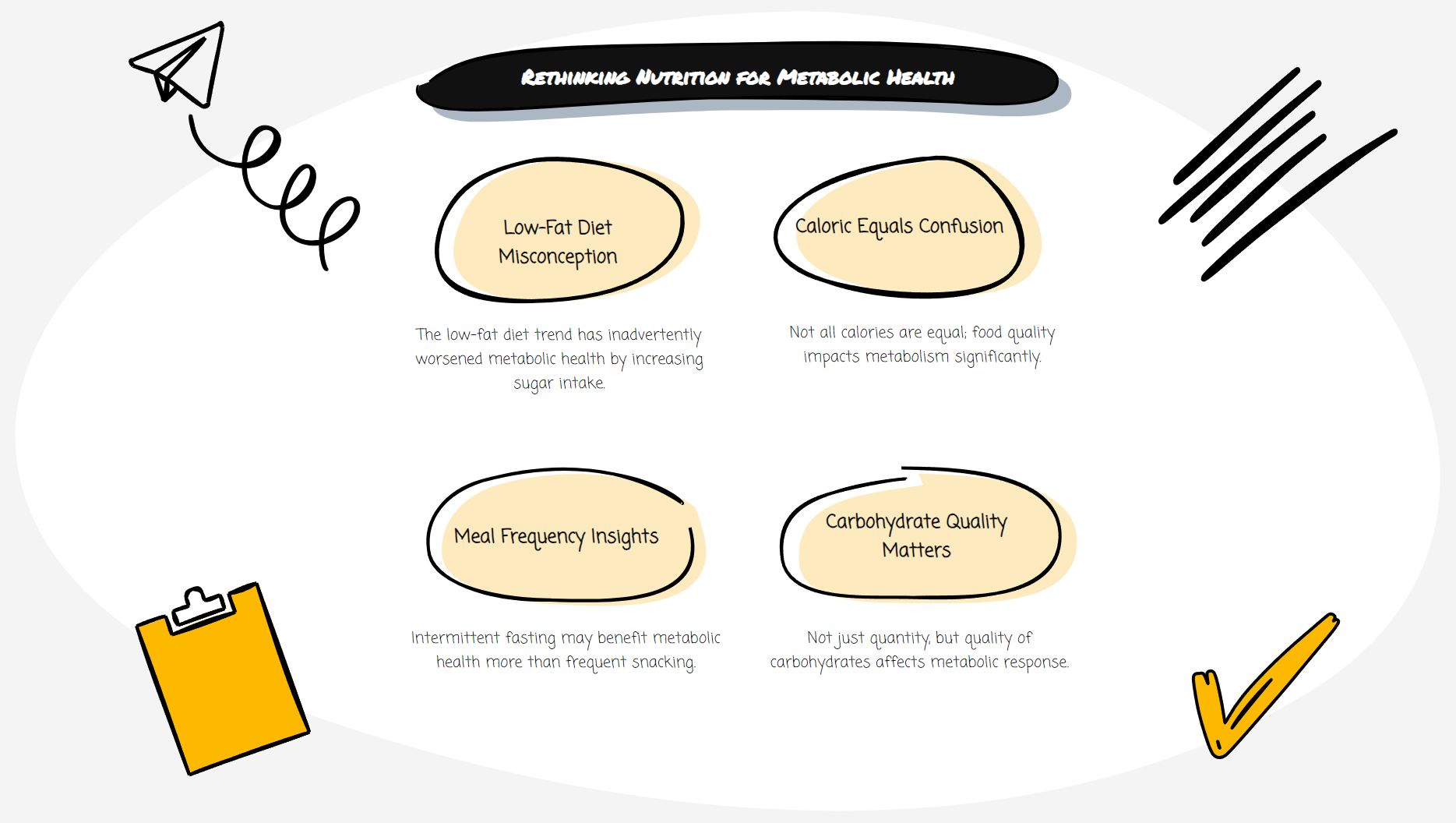
The Low-Fat Fallacy
Since the 1970s, health authorities have championed low-fat diets as the path to heart health and weight management. This recommendation led to an entire industry of low-fat, high-carbohydrate products filling supermarket shelves.
The unintended consequence? As fat consumption decreased, carbohydrate intake increased dramatically. Food manufacturers replaced fat with sugar and refined carbohydrates to maintain palatability, creating a perfect storm for metabolic dysfunction.
Research now indicates that many fats, particularly monounsaturated and omega-3 fatty acids, benefit metabolic health. A 2018 systematic review in the British Medical Journal found that reducing saturated fat intake had no significant effect on cardiovascular mortality.
More troubling, the vilification of dietary fat led many to avoid nutrient-dense foods like eggs, fatty fish, and nuts that contain essential nutrients for metabolic function. The focus on fat reduction rather than food quality has proven misguided.
Calorie Counting Confusion
The "calories in, calories out" model remains the cornerstone of conventional weight management advice. This simplistic approach treats all calories equally, regardless of their source or metabolic impact.
But our bodies process 100 calories of sugar differently than 100 calories of protein or fat. Protein requires more energy to digest and has greater satiety effects. Certain fats support hormone production essential for metabolic regulation. Refined carbohydrates spike insulin levels, promoting fat storage and increasing hunger.
The calorie-counting paradigm also ignores how food quality affects the gut microbiome, which plays a crucial role in metabolism and weight regulation. Despite being calorie-free, emerging research suggests that artificial sweeteners may disrupt gut bacteria and glucose tolerance.
A more nuanced approach recognizes that what we eat fundamentally alters how our bodies function at a cellular level, beyond simple caloric mathematics.
The Meal Frequency Myth
The recommendation to eat small, frequent meals to "stoke your metabolism" has become conventional wisdom. Many healthcare providers still advise patients never to skip meals and to eat regular daily snacks.
This advice contradicts our evolutionary biology. Humans evolved with periods of feast and famine, not constant feeding. Emerging research on intermittent fasting and time-restricted eating suggests that giving our digestive systems regular breaks may improve insulin sensitivity, reduce inflammation, and enhance cellular repair processes.
Constant eating keeps insulin levels elevated throughout the day, potentially contributing to insulin resistance over time. For many individuals, fewer meals with longer gaps between eating periods may better support metabolic health than the grazing pattern commonly recommended.
Carbohydrate Requirements Reconsidered
The foundation of the conventional food pyramid places carbohydrates as the base of our diet, recommending 6-11 servings daily. While carbohydrates are not inherently harmful, this blanket recommendation fails to account for individual metabolic differences and the quality of carbohydrate sources.
People with insulin resistance, prediabetes, or type 2 diabetes often experience improved glycemic control with lower carbohydrate approaches. A 2019 consensus report in Diabetes Care acknowledged that low-carbohydrate eating patterns are among the most studied dietary approaches for type 2 diabetes.
Furthermore, the type of carbohydrate matters significantly. Fiber-rich, nutrient-dense carbohydrates from vegetables, fruits, and legumes affect metabolism differently than refined grains and added sugars. Yet conventional advice often fails to emphasize this crucial distinction.
Beyond One-Size-Fits-All Nutrition
Perhaps the most damaging aspect of conventional dietary advice is its universal application. Human metabolism varies based on genetics, gut microbiome composition, activity levels, health status, age, and numerous other factors.
Research in personalized nutrition suggests that individuals can have dramatically different glycemic responses to identical foods. What constitutes an optimal diet for one person may trigger metabolic dysfunction in another.
The future of nutritional medicine lies not in broad population guidelines but in individualized approaches that consider metabolic individuality. Continuous glucose monitors, microbiome testing, and other emerging technologies are beginning to enable truly personalized nutritional recommendations.
Reclaiming Metabolic Health
Moving beyond conventional nutrition myths requires healthcare providers and individuals to embrace scientific advances in nutritional science. This means:
1. Focusing on food quality rather than simply counting calories or grams of fat
2. Recognizing that metabolic responses to food are highly individualized
3. Considering the timing of meals as well as their content
4. Understanding that dietary needs change throughout life and with different health conditions
5. Questioning nutritional dogma, even when it comes from authoritative sources
The gap between nutritional research and clinical practice remains substantial. Many healthcare providers receive minimal nutrition education during their training, often based on outdated paradigms. Bridging this gap requires ongoing education for medical professionals and greater integration of nutritional science into healthcare.
The path forward for individuals involves becoming informed consumers of food and nutritional information. This doesn't mean rejecting all conventional wisdom but approaching dietary recommendations with healthy skepticism and an awareness of one's metabolic responses.
The metabolic health crisis won't be solved with the same thinking that created it. By questioning conventional nutrition myths and embracing evidence-based, personalized approaches, we can reverse the tide of metabolic dysfunction and create truly nourishing dietary patterns.
