Your Brain Runs on Fat When Glucose Fails
Your Brain Runs on Fat When Glucose Fails
Brains need fuel. When standard options run out, alternative energy sources become crucial survival tools. This metabolic flexibility might be our most underappreciated weapon against cognitive decline.
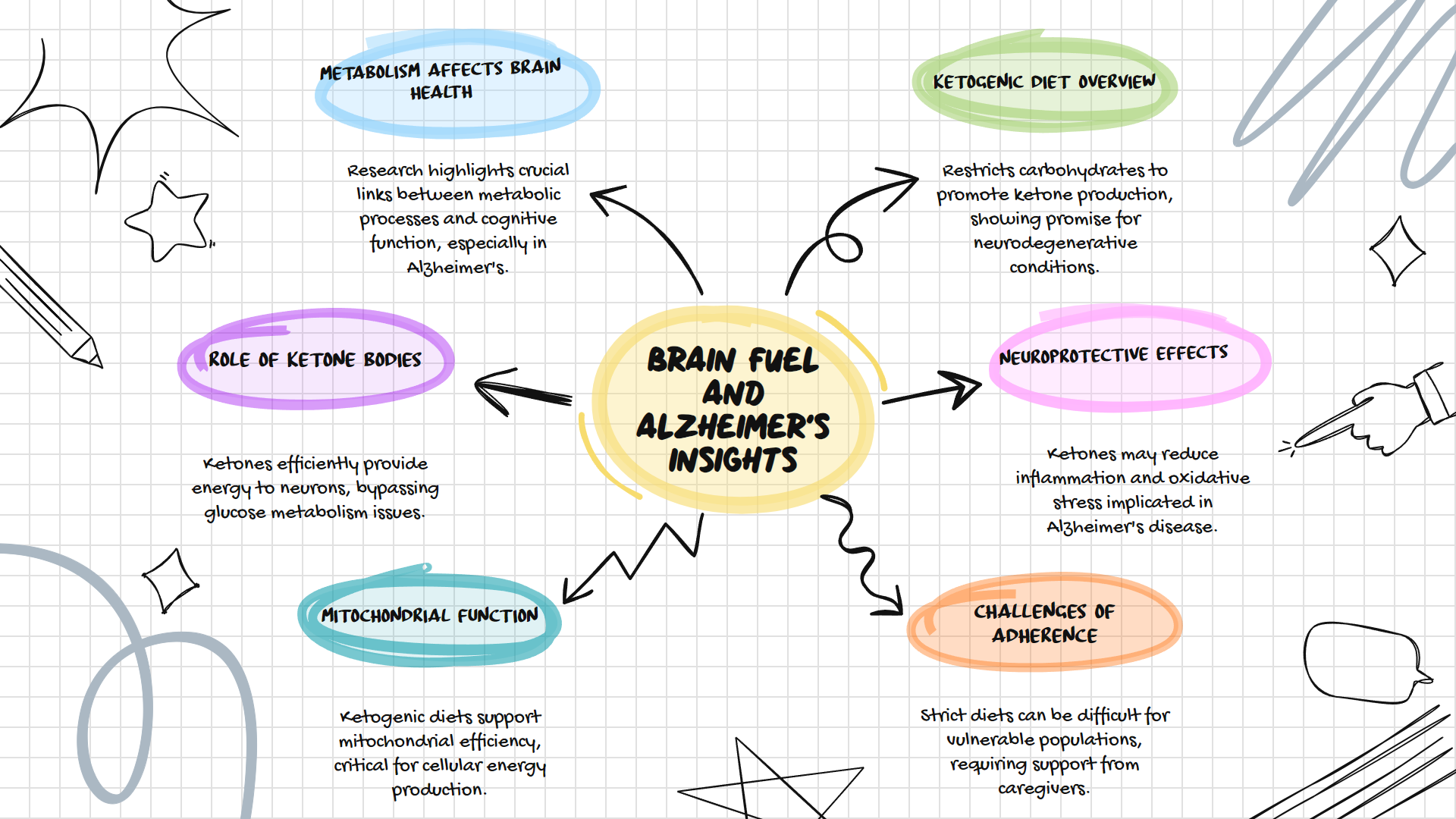
The connection between metabolism and brain health represents one of the most promising frontiers in Alzheimer's research. While pharmaceutical approaches continue to disappoint, a growing body of evidence suggests that how we fuel our brains could fundamentally alter disease progression. The ketogenic diet and resulting ketone bodies offer a metabolic approach that addresses what many researchers now recognize as a core feature of Alzheimer's disease: impaired brain energy metabolism.
The Brain's Energy Crisis
Our brains are energy hogs, consuming roughly 20% of our body's energy while representing only 2% of our body weight. Traditionally, glucose serves as the primary fuel source for brain cells. But what happens when glucose metabolism becomes impaired?
This question sits at the heart of what many researchers call "Type 3 diabetes" or "brain insulin resistance." Brain scans of Alzheimer's patients reveal significant reductions in glucose utilization in several brain regions, often appearing decades before clinical symptoms emerge. This metabolic deficit creates an energy crisis at the cellular level, potentially triggering or accelerating the pathological cascade of Alzheimer's disease.
The brain's inability to efficiently use glucose doesn't just happen alongside Alzheimer's. It may drive disease progression.
Ketones as Alternative Brain Fuel
When glucose availability drops, our bodies produce ketone bodies as an alternative fuel source. These molecules, primarily beta-hydroxybutyrate, acetoacetate, and acetone, are generated in the liver from fatty acids during low-carbohydrate intake or fasting periods.
Unlike glucose, ketones don't require insulin to enter cells. They cross the blood-brain barrier efficiently and provide rapid energy to neurons. Most importantly, research suggests that even in Alzheimer's patients, the brain's ability to utilize ketones remains relatively preserved despite impaired glucose metabolism.
This metabolic pathway offers a potential workaround for the brain's energy crisis. By providing an alternative fuel source, ketones may help compensate for deficits in glucose utilization, potentially slowing or reducing neuronal damage.
The Ketogenic Diet and Brain Health
The ketogenic diet dramatically restricts carbohydrates while emphasizing fats, forcing the body to produce ketones for fuel. Originally developed to treat epilepsy in the 1920s, this dietary approach has demonstrated remarkable efficacy for reducing seizures in drug-resistant cases.
Recent research extends these benefits to neurodegenerative conditions. Small clinical trials have shown improvements in cognitive function when Alzheimer's patients follow ketogenic diets or consume ketogenic supplements. One study demonstrated that elevated ketone levels correlated with improved memory performance in subjects with mild cognitive impairment.
Beyond simply providing alternative fuel, ketones appear to offer neuroprotective benefits. They reduce oxidative stress, decrease inflammation, and may even reduce the production of toxic amyloid proteins associated with Alzheimer's disease.
Beyond Energy Production
The ketogenic diet's benefits extend beyond simply providing alternative fuel. Metabolic ketosis triggers systemic changes that may directly address several pathological processes in Alzheimer's disease:
First, ketones reduce inflammation. Chronic neuroinflammation plays a central role in Alzheimer's progression, and beta-hydroxybutyrate has been shown to block inflammatory pathways in the brain.
Second, ketosis improves mitochondrial function. Mitochondria, our cellular power plants, become dysfunctional in Alzheimer's disease. Ketones enhance mitochondrial efficiency and stimulate the creation of new mitochondria.
Third, ketogenic diets may enhance autophagy, the cellular "cleanup" process that removes damaged proteins and cellular components. This could potentially help clear toxic protein aggregates associated with neurodegeneration.
Practical Limitations and Considerations
Despite promising research, significant challenges remain. Strict ketogenic diets can be difficult to maintain, especially for elderly individuals or those with cognitive impairment. Adherence often requires substantial support from caregivers and healthcare providers.
Additionally, ketogenic diets may not be appropriate for all patients. Those with certain metabolic conditions, pancreatic insufficiency, or fat metabolism disorders may not tolerate high-fat diets. Medical supervision becomes essential when implementing ketogenic approaches in vulnerable populations.
The scientific evidence, while encouraging, remains preliminary. Larger clinical trials are needed to establish definitive benefits and optimal implementation strategies. Questions about timing, duration, and specific dietary compositions remain unanswered.
Future Directions
The metabolic approach to Alzheimer's offers several promising research avenues. Medium-chain triglyceride (MCT) supplements provide a more accessible way to elevate ketone levels without requiring strict dietary adherence. These supplements can rapidly increase blood ketone levels and have shown cognitive benefits in small trials.
Exogenous ketone supplements represent another frontier, allowing patients to achieve ketosis without dietary restriction. These supplements directly provide beta-hydroxybutyrate, potentially offering metabolic benefits without the challenges of dietary change.
Perhaps most exciting is the potential for personalized approaches. Genetic factors, baseline metabolic health, and disease stage likely influence individual responses to ketogenic interventions. Future research may help identify which patients will benefit most from metabolic therapies.
A Paradigm Shift in Treatment
The metabolic approach to Alzheimer's represents a fundamental shift in how we conceptualize and treat neurodegenerative disease. Rather than focusing exclusively on protein aggregates like amyloid and tau, this approach addresses the underlying energetic crisis that may drive pathology.
While not a cure, ketogenic approaches offer a promising adjunctive strategy that addresses a fundamental aspect of Alzheimer's pathophysiology. As research continues to evolve, metabolic interventions may become essential to comprehensive treatment protocols.
The brain's ability to utilize alternative fuel sources provides hope and opens new therapeutic possibilities. By understanding and leveraging these metabolic pathways, we may find ways to preserve cognitive function even as traditional energy systems begin to fail.
