Why High LDL Cholesterol Might Not Be Your Heart's Enemy
Why High LDL Cholesterol Might Not Be Your Heart's Enemy
What if everything you've been told about cholesterol is incomplete?
For decades, we've heard a simple story: high LDL cholesterol clogs arteries and causes heart attacks. This narrative has driven millions of prescriptions for cholesterol-lowering medications and countless low-fat diet recommendations.
But emerging research paints a far more nuanced picture.
The cholesterol and cardiovascular disease relationship appears more complex than conventional wisdom suggests. This complexity becomes particularly evident when examining people following low-carbohydrate diets who develop what researchers call the "lean mass hyper-responder" phenotype.
The Lean Mass Hyper-Responder Paradox
When metabolically healthy individuals adopt low-carbohydrate diets, some experience dramatic increases in their LDL cholesterol. These "lean mass hyper-responders" often show LDL levels well above 200 mg/dL, exceeding conventional safety thresholds.
Yet something curious happens. Despite their elevated LDL, these individuals typically display excellent metabolic health markers: low triglycerides, high HDL cholesterol, normal blood pressure, and optimal blood glucose levels.
This phenomenon raises a critical question: Does high LDL alone predict cardiovascular risk?
Recent research suggests it doesn't. A preliminary study by Dr. Matt Budoff found that people with this profile showed no increase in coronary plaque compared to matched controls with much lower LDL levels, despite having LDL levels nearly 150 mg/dL higher.
Beyond Total LDL: The Particles Matter
To understand this apparent contradiction, we must look deeper than total LDL cholesterol. Not all LDL particles are created equal.
LDL particles come in different sizes and densities. Large, buoyant LDL particles (pattern A) behave differently in the body than small, dense LDL particles (pattern B).
The distinction is crucial. Research shows that small, dense LDL particles are strongly associated with heart disease, while large, buoyant LDL particles show little to no association with heart disease.
Low-carbohydrate diets tend to shift LDL from small, dense to large, buoyant particles. This transformation may explain why some people with high total LDL on low-carb diets don't develop the arterial plaque we would expect under the conventional model.
Triglycerides and HDL: The Ratio That Matters
If LDL alone doesn't tell the full story, what does?
The ratio between triglycerides and HDL cholesterol is a powerful predictor of cardiovascular risk. A triglyceride/HDL ratio above two is considered a significant risk factor, with research showing people with the highest ratio having 16 times the heart attack risk compared to those with the lowest ratio.
This makes intuitive sense when we consider what these markers represent. Elevated triglycerides often indicate excess carbohydrate consumption and metabolic dysfunction. Low HDL typically accompanies insulin resistance and inflammation.
Together, these markers paint a picture of metabolic health that total LDL cannot capture.
Lessons From Familial Hypercholesterolemia
People with familial hypercholesterolemia (FH) provide another fascinating window into the cholesterol-heart disease relationship. These individuals have genetic mutations that cause extremely high LDL cholesterol at birth.
According to conventional wisdom, people with FH should uniformly develop early heart disease. Yet the reality is more complex.
While FH does increase cardiovascular risk, studies of FH populations reveal that many individuals with this condition live long, healthy lives despite decades of elevated LDL.
What distinguishes FH patients who develop heart disease from those who don't? It's not their LDL levels, which are similarly elevated in both groups.
Instead, blood glucose levels, coronary calcium scores, and clotting factors appear to determine who develops heart disease. In multiple studies, FH patients with regular metabolic health markers show cardiovascular risk similar to the general population despite their high LDL.
The Immune Function of LDL
Beyond its role in cholesterol transport, LDL serves another critical function rarely discussed: immune support.
LDL particles help neutralize bacterial toxins and support the immune system's response to pathogens. This protective function may explain observations that elderly people with higher LDL often live longer than those with lower levels.
Studies have found that people with naturally low LDL, as well as those taking statins, show increased susceptibility to severe infections like sepsis. This suggests that artificially lowering LDL may have unintended consequences for immune function.
This immune role represents a significant blind spot in conventional cholesterol discussions.
Clotting Factors: The Missing Link
If LDL isn't the primary driver of cardiovascular events, what is?
Growing evidence points to blood clotting factors as a critical mechanism. Proteins like fibrinogen and factor VIII are essential in blood clot formation and breakdown.
Studies consistently show that elevated clotting factors strongly predict cardiovascular events, independent of LDL levels. This relationship holds across age groups and populations.
In FH patients specifically, those who develop heart disease show higher levels of clotting factors than those who don't, despite identical LDL levels.
This suggests that the formation and breakdown of blood clots, rather than cholesterol accumulation alone, may be the primary mechanism driving heart attacks and strokes.
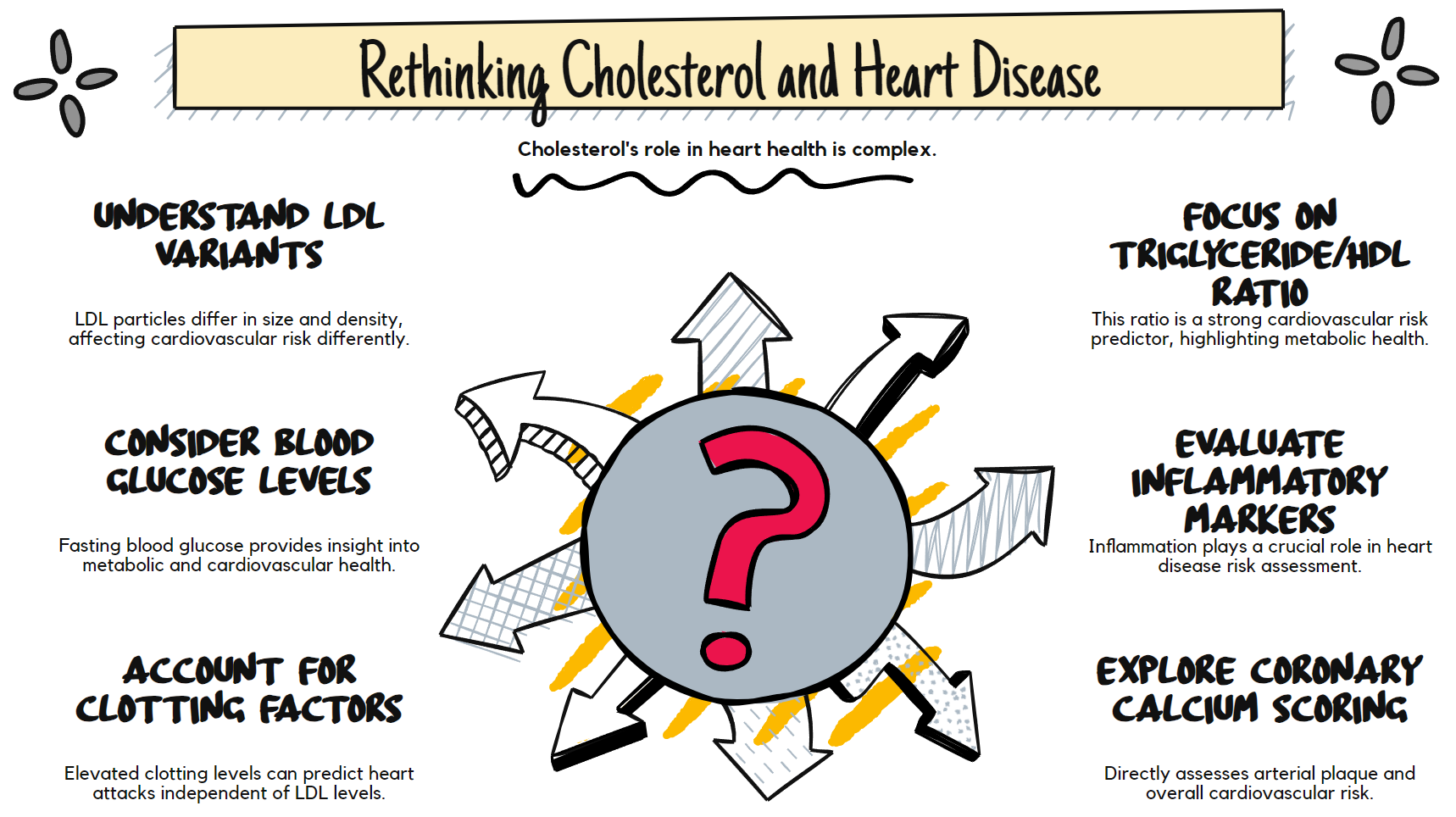
Rethinking Cardiovascular Risk Assessment
These findings demand a more nuanced approach to cardiovascular risk assessment.
Rather than focusing exclusively on LDL cholesterol, a comprehensive evaluation should include:
1. Triglyceride/HDL ratio
2. Fasting blood glucose and insulin levels
3. Blood pressure
4. Inflammatory markers
5. Clotting factors when possible
6. Coronary calcium scoring for direct assessment of arterial plaque
These additional markers provide crucial context for individuals on low-carbohydrate diets who see their LDL rise. If triglycerides are low, HDL is high, and other metabolic markers are optimal, the elevated LDL may not carry the risk traditionally assumed.
Practical Implications
This more nuanced understanding of cholesterol and cardiovascular risk has several practical implications.
First, it suggests that dietary approaches should be evaluated based on their comprehensive metabolic effects, not just their impact on LDL cholesterol. A diet that raises LDL but improves triglycerides, HDL, blood glucose, and inflammation may benefit cardiovascular health.
Second, it highlights the importance of personalized risk assessment. Two people with identical LDL levels may have vastly different cardiovascular risk profiles based on other factors.
Third, it raises questions about the widespread use of LDL-lowering medications in people with otherwise optimal metabolic health. The risk-benefit calculation becomes more complex when considering LDL's immune functions and the limited absolute risk reduction seen in many statin trials.
Beyond Simplistic Models
The cholesterol-heart disease relationship exemplifies how simplistic models often fail to capture biological complexity.
Our understanding continues to evolve as research reveals new layers of nuance. The lean mass hyper-responder phenomenon on low-carbohydrate diets represents a natural experiment that challenges conventional wisdom and opens new avenues for investigation.
This doesn't mean we should ignore LDL cholesterol entirely. It remains one piece of the cardiovascular risk puzzle. But it's time to place it in proper context alongside other markers that may provide more meaningful insights into actual risk.
For individuals concerned about their cardiovascular health, especially those following low-carbohydrate diets, this broader perspective offers reassurance and a roadmap for more comprehensive risk assessment.
The cholesterol and heart disease story isn't as simple as we once thought. By embracing this complexity, we gain a more accurate understanding of cardiovascular risk and more effective prevention strategies.
