Why Fiber Might Not Be Your Digestive Savior
Why Fiber Might Not Be Your Digestive Savior
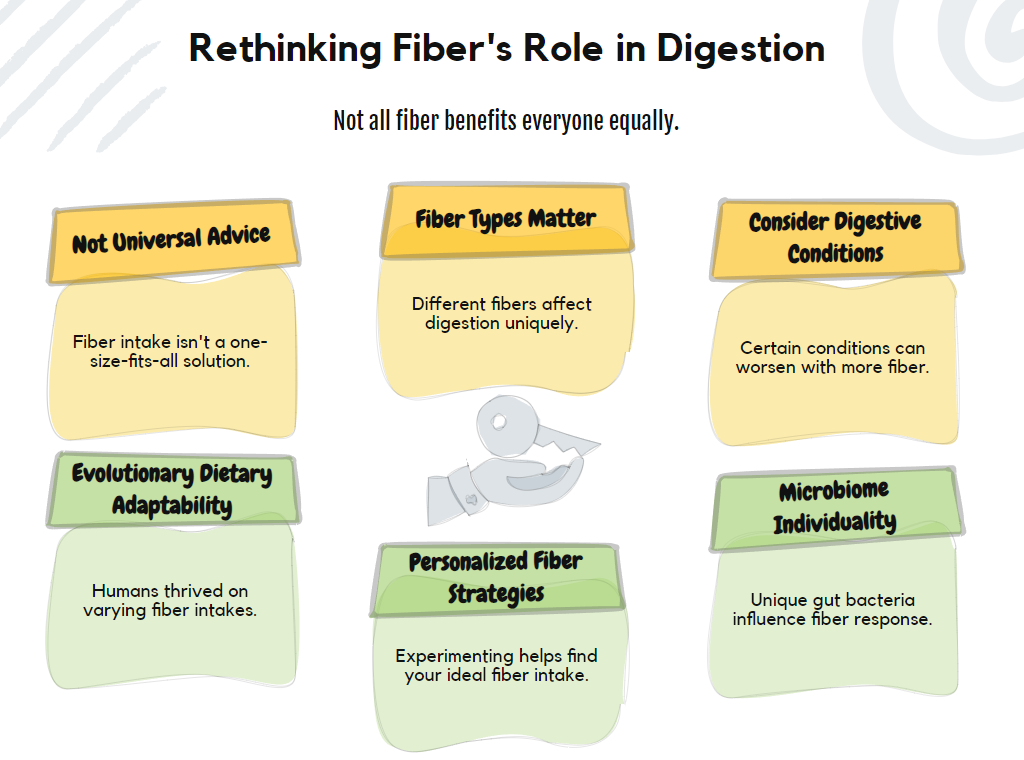
We trust fiber—the golden nutrient for gut health, the digestive hero praised by doctors, dietitians, and wellness influencers alike. But what if this universal recommendation deserves a second look?
For decades, we've been told to increase fiber intake for better digestion, regular bowel movements, and overall gut health. The advice seems simple: eat more fiber, feel better. This recommendation has become so ingrained in the nutritional gospel that questioning it feels almost heretical.
Yet science rarely deals in absolutes, and nutrition science even less so.
The conventional wisdom around fiber deserves scrutiny not because it's wrong, but because it's incomplete. The human digestive system is remarkably complex and individualized. What works for one person might trigger discomfort in another. This nuance gets lost when we reduce digestive health to simplistic fiber-centric recommendations.
When More Fiber Makes Things Worse
The standard "more fiber" advice can backfire spectacularly for people with certain digestive conditions. Those with irritable bowel syndrome (IBS), small intestinal bacterial overgrowth (SIBO), or inflammatory bowel diseases often discover that increasing fiber intake worsens their symptoms rather than improving them.
Consider the low-FODMAP diet, now a standard intervention for IBS sufferers. This approach restricts many high-fiber foods that contain fermentable carbohydrates. For these individuals, the indiscriminate addition of fiber can trigger bloating, pain, and irregular bowel function.
Similarly, during acute flare-ups of Crohn's disease or ulcerative colitis, high-fiber foods can mechanically irritate an already inflamed digestive tract. In these cases, the standard fiber recommendation isn't just unhelpful—it's potentially harmful.
Not All Fiber Is Created Equal
The binary classification of "soluble" versus "insoluble" fiber barely scratches the surface of fiber's complexity. Fibers vary dramatically in their fermentability, viscosity, and effects on gut transit time. Some fibers feed beneficial bacteria, while others primarily add bulk to stool. Some people have slow digestion, while others speed it up.
Research shows that specific fibers have targeted effects on different aspects of digestive function. Beta-glucans from oats and barley have various physiological effects compared to lignins from flaxseeds or pectins from fruits. The prebiotic fibers that nourish beneficial bacteria differ from those that primarily affect stool consistency.
This complexity means that generic recommendations to "eat more fiber" without specifying types, sources, or individual context miss the mark entirely.
The Evolutionary Perspective
Our ancestors didn't consume uniform amounts of fiber across different geographical regions and seasons. Hunter-gatherer societies had varying fiber intakes depending on their environment and food availability. Some thrived on extremely high-fiber diets, while others consumed relatively little plant material during certain seasons.
This suggests that humans evolved with adaptability to different fiber intakes rather than a universal requirement for high amounts. Our digestive systems show remarkable flexibility, which explains why people can thrive on diets ranging from nearly all-animal to predominantly plant-based.
The modern assumption that everyone requires the same high fiber intake ignores this evolutionary adaptability and individual variation.
The Microbiome Factor
Perhaps the most compelling reason to reconsider one-size-fits-all fiber advice comes from microbiome research. Each person harbors a unique community of gut bacteria with different metabolic capabilities and fiber preferences.
Your microbiome composition determines how you respond to different fibers. Some people's gut bacteria efficiently ferment certain fibers, producing beneficial short-chain fatty acids. Others lack the microbial machinery to process the same fibers, leading to gas, bloating, and discomfort.
This microbial individuality helps explain why two people can eat identical fiber-rich meals and experience completely different digestive responses. What feeds one person's beneficial bacteria might feed another's problematic microbes.
Toward Personalized Fiber Recommendations
Rather than asking "How can I eat more fiber?" a better question might be "What types and amounts of fiber work best for my unique digestive system?"
Finding optimal fiber intake requires attention to your body's signals and responses. It means experimenting with different fiber sources and amounts while monitoring your feelings. It might involve temporarily reducing certain fibers before strategically reintroducing them.
This personalized approach acknowledges that digestive health isn't achieved through adherence to universal rules but through discovery of your body's individual needs.
Beyond Fiber Fixation
Digestive health encompasses far more than fiber intake. Stress management, meal timing, chewing thoroughly, staying hydrated, and physical activity all profoundly affect how your digestive system functions. Focusing exclusively on fiber neglects these equally important factors.
The most beneficial approach to digestive wellness integrates fiber considerations within this broader context. Sometimes improving digestion requires addressing stress or sleep rather than adding another serving of bran cereal.
Challenging conventional wisdom doesn't mean rejecting fiber's importance. Instead, it means developing a more sophisticated understanding of how fiber fits into the complex puzzle of digestive health. It means moving beyond simplistic recommendations toward an approach that honors biological individuality and complexity.
The next frontier in digestive health isn't finding the perfect universal fiber recommendation—it's developing frameworks that help each person discover their optimal approach to nourishing their unique digestive system.
