The Ketogenic Revolution Transforming Psychiatry
The Ketogenic Revolution Transforming Psychiatry
The brain runs on glucose. Until it doesn't.
For decades, psychiatric medicine has focused almost exclusively on neurotransmitter manipulation through pharmaceutical interventions. Yet for many patients, these approaches fall short. Treatment resistance remains a stubborn reality across the spectrum of mental health conditions.
What if the most powerful psychiatric medicine isn't a pill but a metabolic state?
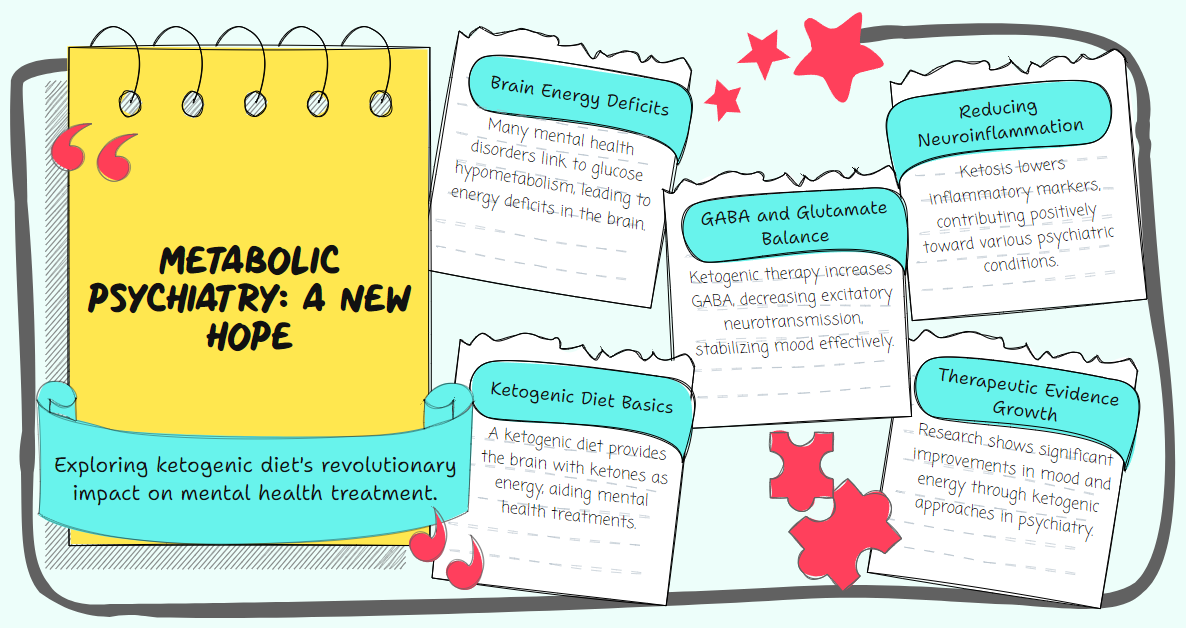
An emerging field called Metabolic Psychiatry is challenging fundamental assumptions about mental illness treatment by focusing on how metabolic processes impact brain function. At its center is a therapeutic approach with a century-old pedigree but revolutionary new applications: the ketogenic diet.
When Brain Fuel Matters
Conventional wisdom holds that the brain requires glucose to function. This is partially true. But the brain can also run efficiently on ketones, molecules produced when the body metabolizes fat instead of carbohydrates.
This metabolic flexibility isn't just a biological curiosity. It may be the key to treating some of our most challenging psychiatric conditions.
Dr. Shebani Sethi, founder of Metabolic Psychiatry at Stanford Medicine, explains that ketogenic therapy provides ketones as an alternative fuel for brains with energy dysfunction. This addresses metabolic deficits that may underlie many psychiatric disorders.
The scientific rationale is compelling. Ketogenic metabolic therapy increases the gamma-aminobutyric acid (GABA) ratio to glutamate in neurons. This balances inhibitory and excitatory neurotransmitters, suppressing the excessive neuronal firing that contributes to mental illness.
Brain glucose hypometabolism appears to be a component of many mental health disorders. When the brain struggles to use glucose efficiently, ketones offer an alternative energy source that bypasses this metabolic roadblock.
From Epilepsy to Psychiatry
The ketogenic diet's therapeutic potential isn't new. It's been used to treat epilepsy for nearly a century.
What's revolutionary is applying this approach to psychiatric conditions. The connection makes biological sense. Many anti-epileptic medications are also used to treat psychiatric disorders, suggesting shared pathophysiological mechanisms.
Several versions of the ketogenic diet have been developed for metabolic therapies, tailored for individual response and therapeutic targets. The classic ketogenic diet comprises approximately 80% fats, 15% proteins, and 5% carbohydrates.
This macronutrient profile induces nutritional ketosis, where the liver produces ketone bodies from fatty acids. These ketones then serve as an alternative energy source for the brain.
Beyond Energy Production
The therapeutic effects of ketosis extend beyond simply providing alternative brain fuel.
Ketogenic diets promote neurotransmitter regulation, reduce neuroinflammation, provide neuroprotection, and address metabolic dysregulation such as insulin resistance. These multiple mechanisms may explain why ketogenic approaches show promise across various psychiatric conditions.
Interestingly, ketogenic approaches may also protect against and ameliorate the side effects of some psychiatric medications known to cause metabolic disorders. This dual benefit addresses both primary psychiatric symptoms and iatrogenic metabolic complications.
The Evidence Emerges
Skepticism is warranted with any new therapeutic approach. But the evidence supporting ketogenic interventions for psychiatric conditions is growing rapidly.
A groundbreaking study by Campbell et al. recruited 26 participants with bipolar disorder and implemented a modified ketogenic intervention over 6-8 weeks. The diet was individually tailored to meet target ketones of 1-4 mmol/L and plasma glucose of 4-7.8 mmol/L.
The results were striking. Ketogenic therapy resulted in 69% of participants showing significant clinical improvement. Researchers observed a positive correlation between daily ketone levels and improvements in mood and energy scores.
For schizoaffective disorder, Laurent et al. investigated the effect of ketogenic metabolic therapy on two individuals who had not responded to standard medication approaches. Both experienced significant improvements over the first 6-8 weeks, with ongoing benefits tracked to 24 weeks.
Most remarkably, both cases achieved remission of their symptoms. At follow-up, medication prescription was either complete or in progress.
When Nothing Else Works
Perhaps the most compelling evidence comes from cases of treatment-resistant conditions that responded to ketogenic interventions after all conventional approaches failed.
Consider the case of a 47-year-old woman with lifelong treatment-resistant major depressive disorder. Her symptoms had been severe and progressive over 25 years, leaving her without energy or ability to handle routine responsibilities.
After starting ketogenic metabolic therapy, her symptoms rapidly improved over 8 weeks. Her PHQ-9 (Patient Health Questionnaire) score dropped dramatically from 25 (severe) to 0 (remission).
The transformation was so profound that she stated, "I'm going back to school to get a master's in nutrition science; the program starts next spring! I feel that my brain is ready to learn new things and that I can start a new career."
Similar case reports exist for treatment-resistant schizophrenia, bipolar disorder, and anxiety conditions. While individual cases cannot prove efficacy for all patients, they provide compelling proof-of-concept for this approach.
Mechanisms of Action
Understanding why ketogenic approaches work requires examining multiple biological mechanisms.
First, ketones provide an alternative energy source for brain cells with impaired glucose metabolism. This addresses the fundamental energy deficit that may underlie many psychiatric conditions.
Second, ketosis alters neurotransmitter production and regulation. The increased GABA-to-glutamate ratio helps balance excitatory and inhibitory neurotransmission, potentially stabilizing mood and reducing anxiety.
Third, ketogenic diets reduce neuroinflammation by lowering inflammatory markers in both the brain and periphery. Chronic inflammation is increasingly recognized as a contributor to many psychiatric conditions.
Fourth, ketosis improves mitochondrial function and increases adenosine triphosphate (ATP) production. This enhanced cellular energy production may support optimal neuronal function.
Finally, ketogenic diets address metabolic dysregulation such as insulin resistance, which is increasingly linked to psychiatric symptoms. Improving metabolic health may directly benefit mental health.
Implementation Challenges
Despite promising results, implementing ketogenic approaches in psychiatric care presents significant challenges.
Dietary adherence requires substantial patient education and support. The ketogenic diet represents a dramatic shift from typical eating patterns and demands careful planning and monitoring.
Medical supervision is essential. The potentiation effects of ketogenic diets in conjunction with psychiatric medications require careful management. Medication dosages often need adjustment as metabolic state changes.
Metabolic monitoring must be consistent. Regular measurement of blood glucose, ketones, and other metabolic parameters helps ensure the maintenance of therapeutic targets.
Healthcare provider education remains a significant barrier. Few psychiatrists receive training in nutritional approaches, and many remain unfamiliar with ketogenic interventions.
A Complementary Approach
Ketogenic interventions should be viewed as complementary to, not replacements for, conventional psychiatric care. The most successful implementations integrate metabolic approaches within comprehensive treatment plans.
For many patients, ketogenic therapy may allow medication reduction rather than elimination. The synergistic effects of appropriate medication and metabolic therapy may provide optimal outcomes.
Individual response varies significantly. Some patients experience dramatic improvements, while others see modest or nonexistent benefits. Personalized approaches that account for individual metabolic differences are essential.
The field requires further research to identify which patients are most likely to benefit from ketogenic interventions. Biomarkers that predict treatment response would significantly advance clinical implementation.
The Future of Metabolic Psychiatry
As research advances, several developments appear likely.
First, more precise therapeutic protocols will emerge. Current approaches often use standard ketogenic diets, but future interventions may target specific metabolic pathways relevant to particular psychiatric conditions.
Second, integration with conventional care will improve. As psychiatrists become more familiar with metabolic approaches, combined treatment strategies will become more sophisticated.
Third, technological support will enhance implementation. Continuous glucose monitoring, ketone tracking, and other technologies make metabolic therapy more accessible and precisely targeted.
Finally, preventive applications may develop. Metabolic interventions might help prevent psychiatric symptoms in high-risk individuals by addressing underlying metabolic dysfunction before clinical symptoms emerge.
A Paradigm Shift
Metabolic psychiatry represents more than just a new treatment approach. It signals a fundamental shift in how we understand mental illness.
By recognizing the brain as a metabolic organ whose function depends on energy production and utilization, we open new avenues for intervention. The distinction between "psychiatric" and "metabolic" conditions begins to blur.
This integration of metabolism and mental health reconnects psychiatry with the rest of medicine. It acknowledges that the brain doesn't exist in isolation from the body's metabolic processes.
Metabolic psychiatry offers new hope for patients who have struggled with limited benefit from conventional approaches. While not a panacea, it expands our therapeutic toolkit in meaningful ways.
The most promising aspect may be the potential for addressing root causes rather than merely managing symptoms. By correcting fundamental metabolic dysfunctions, ketogenic approaches may offer more durable improvements than symptom-focused interventions alone.
As research continues and clinical experience grows, metabolic psychiatry will likely become an increasingly important component of comprehensive mental health care. The revolution has only just begun.
