The Gut Revolution in Mental Health Treatment
The Gut Revolution in Mental Health Treatment
Minds change slowly. Science moves forward. But paradigms? They resist transformation until evidence becomes overwhelming.
For over a century, psychiatry has focused almost exclusively on the brain as the source and solution for mental health disorders. Medications target neurotransmitters. Therapies aim to rewire neural pathways. Brain scans search for structural abnormalities. This brain-centric model has dominated our understanding so completely that questioning it seemed almost heretical.
But what if we've been looking in the wrong place?
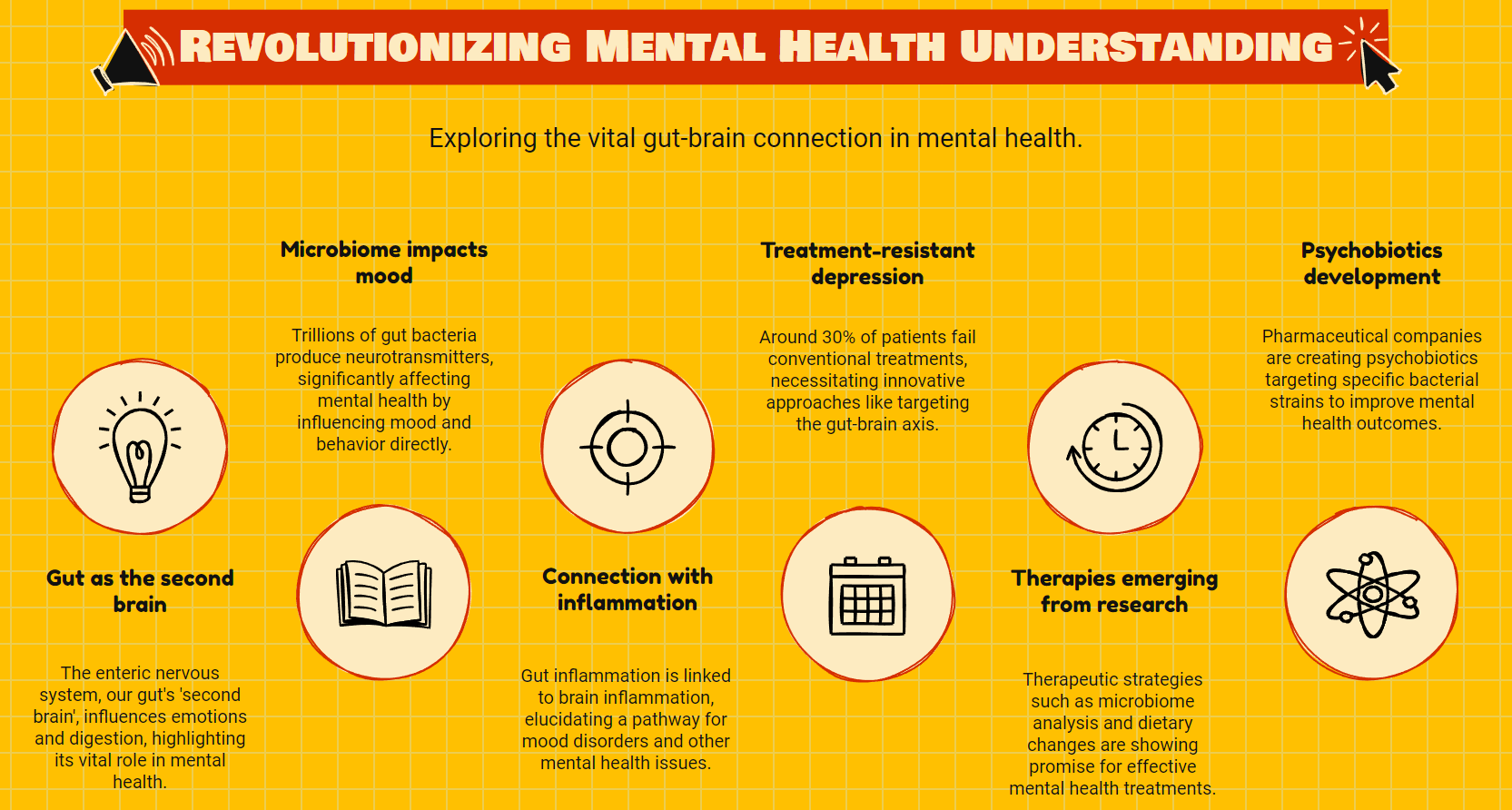
Growing evidence suggests that the gut, not the brain, may be mental health's most promising therapeutic frontier. This isn't merely about the "gut feeling" we experience during anxiety. It's about a complex bidirectional communication system between our intestinal tract and central nervous system that influences mood, cognition, and mental wellbeing at fundamental levels.
The Second Brain in Your Belly
Your digestive system houses what scientists call the enteric nervous system (ENS), a complex network of more than 100 million nerve cells lining your gastrointestinal tract. This "second brain" operates with remarkable independence, controlling digestion and sending signals to the brain that directly affect feelings of sadness, stress, and happiness.
More striking still is the gut microbiome, those trillions of bacteria colonizing your intestines. These microscopic residents produce neurotransmitters like serotonin, dopamine, and GABA. In fact, about 95% of your body's serotonin, often called the "happiness molecule," is manufactured in the gut, not the brain.
The implications are profound. Depression, anxiety, bipolar disorder, schizophrenia, autism spectrum disorders, and even neurodegenerative conditions show consistent patterns of microbiome disruption. Correlation doesn't prove causation, but animal studies demonstrate that transferring gut bacteria from depressed humans to germ-free mice can induce depressive behaviors in previously healthy animals.
Challenging a Century of Dogma
The current psychiatric model emerged in the early 20th century, when the brain became medicine's final frontier. Freud's psychoanalysis gave way to biological psychiatry. The discovery of psychiatric medications in the 1950s cemented the neurotransmitter hypothesis of mental illness. Pharmaceutical companies built empires around drugs targeting brain chemistry.
This approach has helped millions. But it has failed millions more. Treatment-resistant depression affects roughly 30% of patients. Many others experience partial responses or intolerable side effects. The limitations of our brain-only approach have become increasingly apparent.
Meanwhile, epidemiological data shows skyrocketing rates of both gastrointestinal and mental health disorders in Western societies. The connections between inflammatory bowel diseases and psychiatric conditions are so strong that gastroenterologists routinely screen for anxiety and depression. Patients with irritable bowel syndrome are 3-4 times more likely to have anxiety or depression than the general population.
Communication Highways
The gut and brain communicate through multiple pathways. The vagus nerve serves as a direct physical connection, transmitting signals in both directions. The immune system acts as another communication channel, with gut inflammation triggering brain inflammation. Metabolites produced by gut bacteria enter the bloodstream and cross the blood-brain barrier, directly influencing neural function.
This communication network explains why antibiotics can trigger psychiatric side effects, why probiotics show promise for anxiety, and why dietary interventions sometimes succeed where medications fail. The gut-brain axis represents not a rejection of neuroscience but its necessary evolution.
From Theory to Treatment
Therapeutic approaches targeting the gut-brain axis are rapidly moving from fringe to mainstream. Microbiome analysis, once exotic, is becoming standard in integrative psychiatric practices. Specific bacterial strains show promise for specific conditions. Lactobacillus and Bifidobacterium species demonstrate anxiolytic and antidepressant effects in both animal models and human trials.
Fecal microbiota transplantation, already standard for certain gastrointestinal infections, is being studied for psychiatric applications. Dietary interventions focusing on anti-inflammatory, microbiome-supporting patterns show benefits for depression comparable to medication in some studies. Prebiotics and probiotics are being formulated specifically for neuropsychiatric conditions.
The pharmaceutical industry has noticed. Major companies are developing "psychobiotics," precisely targeted bacterial interventions for mental health. Others focus on the metabolites produced by beneficial bacteria. This represents not just new products but a fundamental shift in how we conceptualize mental health treatment.
The Integrated Future
The most promising approach isn't replacing brain-focused treatments with gut-focused ones. It's integrating them. Understanding mental health through the lens of the gut-brain axis allows for more personalized, effective interventions. A patient with inflammation-driven depression might need different treatments than someone with neurotransmitter deficiencies.
This paradigm shift faces resistance. Medical specialties remain siloed. Psychiatrists rarely receive significant training in gastroenterology or nutrition. The research, while compelling, remains incomplete. Questions about which interventions work best for which patients require larger, longer studies.
Yet the direction is clear. We're moving toward a more holistic understanding of mental health that acknowledges the brain's importance without limiting our focus to it alone. The gut represents not just another treatment target but a fundamental reconceptualization of mental illness itself.
Our minds don't exist in isolation within our skulls. They extend throughout our bodies, influenced by and influencing every system. The gut-brain revolution isn't diminishing psychiatry but expanding it, opening new possibilities for millions who have found limited relief from conventional approaches.
The most transformative ideas often seem obvious in retrospect. Perhaps in another century, we'll wonder how we ever thought we could treat the mind without addressing the gut. Until then, this frontier remains both promising and challenging, inviting us to reconsider what we thought we knew about mental health and illness.
