Ketones Unlock New Hope for Failing Hearts
Ketones Unlock New Hope for Failing Hearts
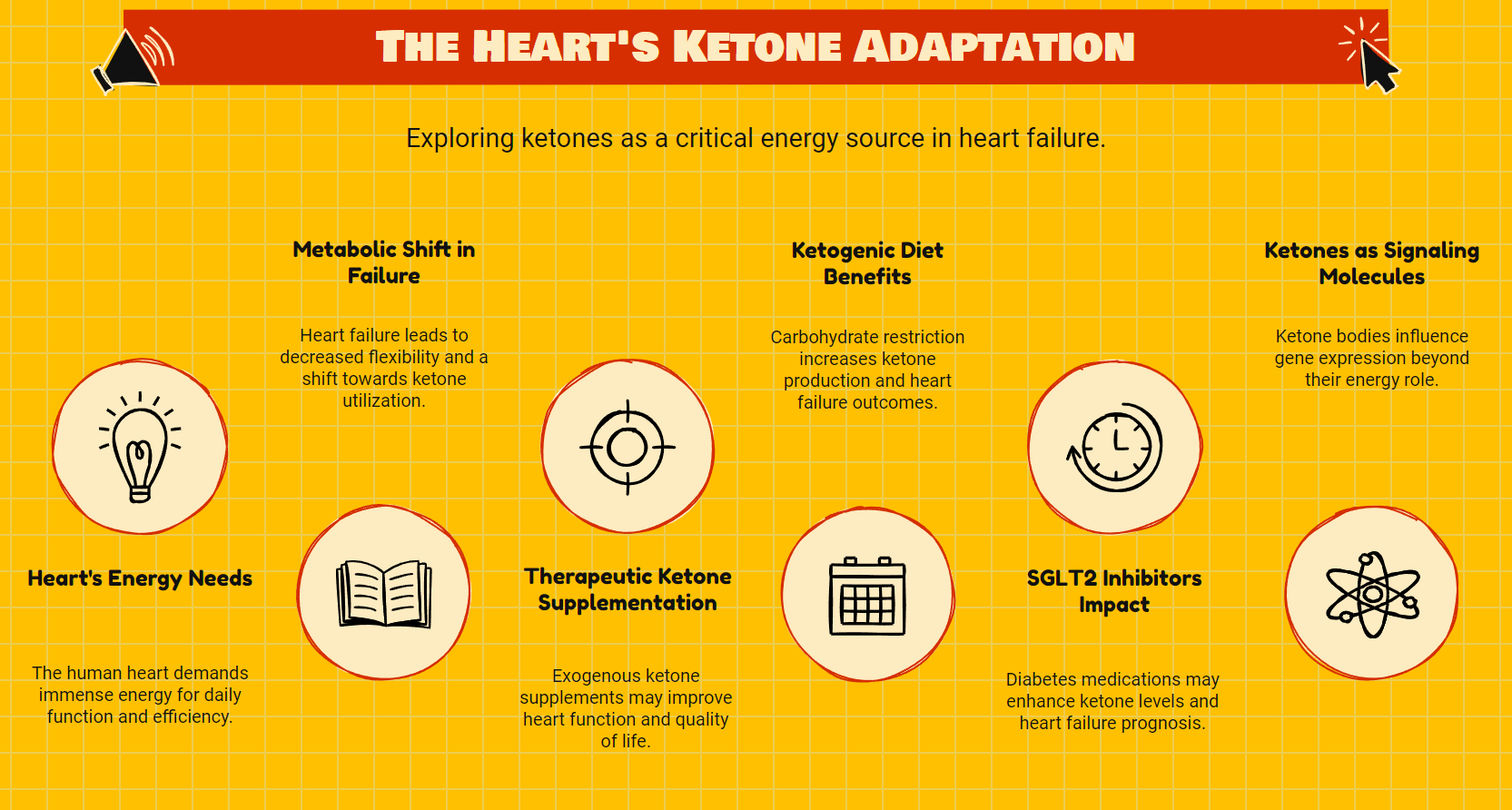
The failing heart doesn't just weaken. It fundamentally changes what it eats.
This metabolic shift represents one of the most promising frontiers in heart failure research. As cardiac function declines, the heart desperately seeks alternative fuel sources—and ketone bodies appear increasingly vital to this survival strategy.
Recent research reveals that this metabolic adaptation isn't merely a consequence of heart failure. It may be a critical protective mechanism that could transform treatment approaches for millions of patients worldwide.
The Heart's Enormous Energy Demands
The human heart beats approximately 100,000 times daily, requiring more energy per gram than any other organ. This metabolic powerhouse consumes about 6 kg of ATP (adenosine triphosphate) daily—enough energy to drive a truck for 20 miles.
To meet these extraordinary demands, the healthy heart maintains remarkable metabolic flexibility. It can readily switch between fatty acids, glucose, lactate, amino acids, and ketone bodies depending on availability and conditions.
Under normal circumstances, fatty acid oxidation provides 60-90% of cardiac energy, with glucose and other substrates making up the difference. Ketones typically contribute minimally unless their circulating levels increase during fasting or carbohydrate restriction.
But heart failure changes everything.
Metabolic Remodeling in the Failing Heart
When the heart begins to fail, it undergoes profound metabolic remodeling. This process involves decreased fatty acid oxidation, impaired glucose utilization, and—critically—increased reliance on ketone bodies as an alternative energy source.
This shift isn't random. The failing heart loses its metabolic flexibility and becomes increasingly dependent on ketones for survival.
Why does this happen? The answer lies in ketones' unique bioenergetic properties.
Ketone bodies provide more ATP per unit of oxygen consumed than glucose or free fatty acids. For the oxygen-starved failing heart, this represents a crucial efficiency advantage. The heart essentially switches to a more economical fuel when its resources become limited.
This adaptive mechanism suggests that increasing ketone availability could potentially support cardiac function during heart failure—a hypothesis now supported by growing clinical evidence.
The Therapeutic Potential of Ketones
The recognition that ketones serve as a preferred fuel source in the failing heart has sparked intense interest in therapeutic applications. Several approaches have emerged to leverage this metabolic pathway:
Exogenous Ketone Supplementation
The most direct intervention involves providing ketones through supplementation. Recent clinical trials demonstrate that 14-day ketone ester treatment in patients with heart failure with reduced ejection fraction (HFrEF) significantly improved cardiac output and reduced pulmonary capillary wedge pressure both at rest and during exercise.
These findings represent concrete cardiovascular benefits that could translate to improved quality of life and reduced hospitalizations for heart failure patients.
Beyond simply providing an alternative fuel source, ketone bodies appear to offer multiple cardioprotective mechanisms:
- Reduced oxidative stress and inflammation
- Prevention of microvascular thinning and loss
- Promotion of vasodilation
- Protection against maladaptive cardiac remodeling
These effects suggest ketones function not just as a fuel but as signaling molecules with broader therapeutic implications.
Ketogenic Diets
Nutritional ketosis through carbohydrate restriction represents another approach to increasing ketone availability. Studies using ketogenic diets in patients with obesity and heart failure have shown promising safety profiles and reduced rates of heart failure hospitalization.
This dietary approach offers several advantages, including sustainability, patient autonomy, and additional metabolic benefits beyond ketone production. However, it requires significant lifestyle modification and careful medical supervision, particularly for patients with complex comorbidities.
SGLT2 Inhibitors
Perhaps most intriguing is the connection between SGLT2 inhibitors and ketone metabolism. This class of diabetes medications has shown remarkable benefits in heart failure partially through their ability to increase circulating ketone levels.
Originally developed to lower blood glucose by promoting urinary glucose excretion, SGLT2 inhibitors unexpectedly demonstrated substantial cardiovascular benefits, reducing heart failure hospitalizations by 25-35% in major clinical trials.
Researchers now believe these benefits stem partly from the drugs' ability to induce mild ketosis, effectively mimicking aspects of fasting metabolism. This creates potential for synergistic therapeutic approaches combining SGLT2 inhibitors with other ketone-enhancing strategies.
Beyond Fuel: Ketones as Signaling Molecules
The therapeutic potential of ketones extends beyond their role as an alternative fuel source. Emerging research suggests ketone bodies function as important signaling molecules that influence gene expression through epigenetic mechanisms.
β-hydroxybutyrate, the primary circulating ketone body, can inhibit class I histone deacetylases and promote the expression of genes involved in antioxidative stress responses. This suggests ketones may reprogram cardiac metabolism at the genomic level, potentially reversing some pathological changes associated with heart failure.
This dual role as both fuel and signaling molecule makes ketones particularly promising therapeutic targets. Few interventions can simultaneously address both the energetic crisis and the maladaptive remodeling that characterize heart failure.
Clinical Implementation Challenges
Despite growing evidence supporting the therapeutic potential of ketones in heart failure, several challenges must be addressed before widespread clinical implementation:
Safety Considerations
While nutritional ketosis differs fundamentally from ketoacidosis, careful monitoring remains essential, particularly in patients with diabetes or those taking certain medications. The distinction between beneficial ketosis and pathological ketoacidosis must be clearly understood by healthcare providers.
Patients taking SGLT2 inhibitors require particularly careful management if ketogenic interventions are considered. A phase 1 clinical trial has demonstrated that combined approaches are possible under expert medical supervision, but this requires specialized knowledge and monitoring protocols.
Delivery Methods
The optimal method for increasing ketone availability remains unclear. Exogenous ketone supplements provide precise dosing but may be expensive and have palatability issues. Ketogenic diets offer broader metabolic benefits but require significant lifestyle changes and nutritional expertise.
Finding the right approach for individual patients will likely require personalized assessment of comorbidities, preferences, and treatment goals.
Integration with Existing Therapies
Heart failure management typically involves multiple medications targeting different pathophysiological mechanisms. Understanding how ketone-enhancing strategies interact with standard heart failure therapies represents a critical research need.
Preliminary evidence suggests potential synergy with SGLT2 inhibitors, but comprehensive studies examining interactions with beta-blockers, ACE inhibitors, and other standard therapies are still needed.
Future Research Directions
Several key questions must be addressed to fully realize the therapeutic potential of ketones in heart failure:
- What is the optimal level of ketosis for cardioprotection?
- Which patient subgroups are most likely to benefit from ketone-enhancing strategies?
- How do ketones interact with traditional heart failure medications?
- What are the long-term effects of therapeutic ketosis on cardiac function and remodeling?
- Can ketone metabolism be enhanced directly in cardiac tissue without systemic ketosis?
Answering these questions will require coordinated efforts across basic science, translational research, and clinical trials. The potential rewards justify this investment, as even modest improvements in heart failure outcomes would represent significant public health benefits.
Practical Implications for Clinicians
While research continues, clinicians should consider several practical implications of current knowledge:
Awareness of metabolic adaptation: Understanding that the failing heart increasingly relies on ketones can inform monitoring and treatment decisions. Clinicians should recognize that metabolic support may be as important as hemodynamic management in some patients.
Nutritional considerations: For appropriate patients, supervised carbohydrate restriction may offer benefits beyond traditional dietary recommendations. Consultation with dietitians familiar with therapeutic carbohydrate reduction can help implement safe and effective nutritional strategies.
Medication selection: The cardiovascular benefits of SGLT2 inhibitors may partially reflect their ketogenic effects. This mechanism should be considered when selecting glucose-lowering therapies for diabetic patients with or at risk for heart failure.
Patient education: Patients increasingly seek information about metabolic approaches to chronic disease. Clinicians should be prepared to discuss the emerging evidence for ketones in heart failure while emphasizing the importance of medical supervision.
The Metabolic Paradigm Shift
The growing recognition of ketones' importance in heart failure represents part of a broader paradigm shift in cardiovascular medicine. Increasingly, heart failure is understood not just as a hemodynamic disorder but as a complex metabolic disease.
This perspective opens new therapeutic avenues beyond traditional approaches focused on contractility, preload, and afterload. By addressing the fundamental bioenergetic crisis underlying heart failure, metabolic interventions like therapeutic ketosis may complement existing treatments to improve outcomes.
The heart's metabolic adaptation to failure—turning to ketones when other fuels become limited—appears to be an intrinsic protective mechanism. Clinical interventions that support and enhance this natural process align with the body's own survival strategies rather than imposing external solutions.
Conclusion
The role of ketone bodies in heart failure represents one of the most promising frontiers in cardiovascular medicine. From their function as an efficient alternative fuel source to their broader signaling effects, ketones offer multiple mechanisms to support the failing heart.
While more research is needed to optimize therapeutic approaches, the evidence increasingly suggests that metabolic interventions targeting ketone metabolism could significantly improve outcomes for heart failure patients.
The failing heart's shift toward ketone utilization isn't merely a consequence of disease—it's a window into potential solutions. By understanding and supporting this adaptive response, clinicians may soon have powerful new tools to address one of medicine's most challenging conditions.
As research progresses, the whispers of the failing heart about its preferred fuel may grow into clear directions for transformative therapies.
